lifestyle
How Does Semaglutide Work To Support Lasting Weight Management?

The calendar flips to a new year, and for many, it’s the familiar moment of reflection: “This is the year I finally stick to my plan.” Resolutions are made, meal plans are printed, workouts are scheduled, but by mid-January, progress stalls. Cravings sneak in, energy dips, and the scale barely budges. The frustration isn’t laziness, it’s biology pushing back, quietly undermining even the most disciplined plans. That’s where Semaglutide comes in. This GLP-1 receptor agonist works with your biology to reduce appetite, slow gastric emptying, and shift metabolism, making weight loss and long-term maintenance achievable rather than a daily battle of willpower. In this article, we’ll break down exactly how Semaglutide works, what to expect from dosing and injections, typical side effects, and what clinical trials reveal about safety and effectiveness.
To make the process easier, MeAgain’s GLP-1 app provides clear guidance, tracks your progress and symptoms, and connects you with care so you can use Semaglutide safely—and finally see lasting results.
Summary
Semaglutide reduces appetite by activating GLP-1 receptors in brain satiety centers, a mechanism that, in trials, has been associated with an average weight loss of 14.9% over 68 weeks.
By slowing gastric emptying, semaglutide extends post-meal fullness and changes meal timing, and clinical protocols typically reach final maintenance dosing in about 17 weeks.
For people with diabetes, semaglutide improves glycemic control, with studies reporting an average HbA1c reduction of approximately 1.5% after six months, reflecting glucose-dependent insulin secretion and a lower risk of hypoglycemia.
Conventional dieting often leads to weight regain: approximately 95% of people regain lost weight within 1 to 5 years. Semaglutide trials showed an average weight loss of approximately 15%, indicating that the medication alters baseline physiology but typically requires ongoing support to sustain results.
Broader clinical effects influence prescribing decisions, as some analyses report a 25% reduction in cardiovascular risk among people using semaglutide, which informs benefit-risk assessments beyond weight alone.
About 70% of patients using semaglutide reported significant weight loss. Still, the best outcomes in trials occurred when medication was paired with structured routines, regular logging, and clinician-guided titration to preserve lean mass and manage side effects.
This is where MeAgain's GLP-1 app fits in: it centralizes injection schedules, hydration and protein targets, and symptom logs, so clinicians and patients can see trends and make safer, data-informed titration decisions.
Table of Contents
Why Weight Loss Isn’t Just About Willpower (and How Semaglutide Works Differently)
How Semaglutide Works in the Brain, Gut, and Blood Sugar Regulation
What Semaglutide Actually Changes Over Time (and What It Doesn’t)
Who Semaglutide is Typically Used for (and Why Support Tools Matter)
Download our GLP-1 app to Turn Your Weight Loss Journey into Your Favorite Game
Why Weight Loss Isn’t Just About Willpower (and How Semaglutide Works Differently)

Worked with many patients over the years, and one pattern always stands out. Take Lisa, a 38-year-old professional who diligently followed meal plans, logged every workout, and tried to control portions with extreme discipline. Yet week after week, the scale barely budged. By Friday evening, she would glance at her notes, see the same stubborn number, and feel the familiar sinking thought: “It must be me I’m failing.”
Why Physiological Resistance Trumps Willpower
What Lisa and so many others experience is not a moral lapse. It’s biology. Hunger is regulated by a network of hormones and neural circuits designed to maintain energy balance. Leptin and ghrelin signal fullness and hunger, while reward circuits in the brain reinforce food-seeking behavior. When calorie intake drops, these systems push back: appetite rises, cravings intensify, and metabolism slows. Conventional dieting fights these mechanisms, which is why long-term adherence often fails. New Leaf Online reports that roughly 95% of people regain weight within 1–5 years.
The GLP-1 Mechanism for Appetite Control
This is where Semaglutide works differently. Rather than trying to override these biological signals with sheer discipline, it works with them. Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist that acts on appetite centers in the brain and slows gastric emptying. The result: fullness arrives sooner, cravings weaken, and the body’s energy signals realign to support weight loss and long-term maintenance.
Appetite Suppression and Behavioral Stabilization Through Dose Titration
In clinical practice, patients like Lisa report that, after proper dose titration, chronic mid-afternoon hunger and intrusive snack urges noticeably decrease. Meal intake becomes steadier throughout the day, and food choices often shift naturally toward balanced portions. Over six months of monitoring, we observed consistent patterns: those who adhered to dose schedules experienced not only lower appetite but also fewer emotional spikes around eating.
Why Does It Make You Feel Full Longer?
Semaglutide slows gastric emptying, allowing food to remain in the stomach longer so satiety signals persist. This simple physical mechanism affects both meal timing and perceived portion size. Meals feel more satisfying without increasing calorie intake. Practical application matters: aligning dose timing with meals, staying hydrated, and tracking protein intake reinforce the fullness window while supporting muscle preservation. For Lisa, integrating these routines transformed her approach to meals from a constant battle into a predictable, manageable system.
Can I Take It With Other GLP-1 Medications?
No. Semaglutide should not be combined with other semaglutide-containing products such as Ozempic or Rybelsus, or other GLP-1 receptor agonists. Overlapping therapies increase risk without providing additional benefit. Switching medications should always be coordinated with your prescriber, and progress, including side effects, should be logged in a reliable tracker to ensure smooth transitions and minimize missed doses.
How Long Do the Results Last, and Should It Be Ongoing
Clinical trials indicate that Semaglutide is intended for sustained use when effective. Long-term studies show meaningful, sustained weight reduction; in 2025, Scientific American reported an average weight loss of 15% for participants on Semaglutide, far exceeding that achieved with most behavioral interventions alone.
Why Translate These Mechanisms Into Routines
Most people, including Lisa at first, rely on sticky notes or mental checklists to manage medication and habits. These low-friction methods feel familiar but often fail when dose schedules, hydration goals, or side-effect notes are scattered across apps or in memory. Anxiety, missed doses, and frustration follow. Platforms like MeAgain centralize injection timing, hydration, protein targets, side-effect logs, and visual progress tracking. This approach ensures doses align with appetite shifts, nutrition supports muscle, and minor adverse effects are caught early, turning scattered effort into measurable, consistent action. Lisa found that once her habits were organized in this way, adherence became effortless, and progress was visible.
What About Side Effects and How to Track Them?
Semaglutide commonly causes mild nausea, early satiety, or stomach upset during dose escalation. Tracking the timing of symptoms relative to injections helps clinicians adjust titration schedules accurately. Recording simple metrics, water intake, protein grams, and injection timing removes guesswork and transforms uncertainty into clear patterns to act on, replacing anxiety with actionable insight.
A Practical Analogy
Semaglutide does not hold your hand at the dinner table. Instead, it subtly reprograms the kitchen signals, helping your appetite naturally switch off at a reasonable hour, cravings diminish, and meals feel satisfying. But the objective complexity and the true advantage lie deeper: the interplay of brain, gut, and blood sugar shifts the entire weight-loss landscape. Understanding these mechanisms allows you, like Lisa, to work with your biology rather than against it.
Related Reading
How Long Does Semaglutide Stay in Your System
What Is Compounded Semaglutide
Should I Take Semaglutide on an Empty Stomach
Does Semaglutide Cause Constipation
Why Does Semaglutide Cause Nausea
How Long Does It Take to See Results From Semaglutide
Does Semaglutide Make You Tired
Does Semaglutide Show Up in Blood Work
How Much Does Semaglutide Cost
How Does Semaglutide Work
How Semaglutide Works in the Brain, Gut, and Blood Sugar Regulation
Hunger is a conversation, not a command. When that conversation gets noisy, mismatched timing, muted satiety cues, surprise blood sugar dips, you feel constant want, not simple appetite. Semaglutide helps those signals arrive more reliably, quieting the background static so decisions about food feel less like willpower and more like listening.
How Do the Brain, Gut, and Blood Sugar Normally Speak to Each Other?
Under normal conditions, the gut sends a chorus of chemical and neural notes after you eat.
Vagal afferents carry rapid mechanical and stretch feedback to the brainstem.
Hormones such as peptide YY and GLP-1 provide a metabolic context.
Circulating glucose, insulin, and leptin tune hypothalamic circuits that gate hunger and reward.
Those signals synchronize meal timing, portion size, and the post-meal slowdown in appetite, forming a short, clear message: stop when enough has arrived.
What Happens When That Communication Breaks Down?
This pattern occurs consistently when meal timing is irregular or when insulin and leptin signaling are blunted: the brain receives mixed signals, so the hedonic reward centers amplify food cues even while homeostatic inputs are weak. Clinically, that looks like waking for night snacks despite having eaten dinner, or feeling compelled to eat after small blood sugar dips. The result is mental noise around food, intrusive cravings, constant attention to availability, and exhaustion from trying to manage every eating moment.
How Does Semaglutide Change that Signal Timing and Clarity?
Semaglutide lengthens and steadies one of the gut’s hormonal notes, so the brain receives a clearer, sustained satiety signal rather than short, inconsistent pulses. That shift reduces the frequency and intensity of intrusive urges; people describe it as the difference between a smoke alarm that keeps chirping and one that only sounds when there is real smoke. The change is not suppression by force; it is correction by timing: fewer false alarms, more reliable “I’m satisfied” messages.
How Semaglutide Aids Weight Loss
Semaglutide exerts prolonged central nervous system effects, influencing satiety networks, thermogenesis, blood pressure regulation, neurogenesis, and inflammation reduction. Because it remains in circulation longer, the drug sustains GLP-1 receptor activation in brain areas that shape meal size and food valuation, while also altering peripheral metabolism. In pancreatic beta cells, GLP-1 receptor engagement boosts glucose catabolism and insulin secretion through the mTOR-dependent HIF-1α pathway, facilitating glycolysis and more robust insulin release; that insulin release often shows a quick peak about 10 minutes after a glucose stimulus, followed by a more extended phase from most insulin granules that can persist for up to 60 minutes.
Semaglutide’s effect is reinforced by:
Slowing DPP-4 action
Prolonging GLP-1 receptor signaling
Activating AMPK pathways that promote GLUT4 translocation to the plasma membrane
5 Ways Semaglutide Promotes Weight Loss
1. Appetite Regulation
Semaglutide steadies hypothalamic satiety circuits, lowering the baseline drive to seek food. Practically, that means smaller, fewer spontaneous snacks. Track meal injection timing and protein intake to align the drug’s peak effect with planned eating windows, so fullness aligns with your daily routine.
2. Delayed Gastric Emptying
By slowing the movement of food from the stomach to the intestine, semaglutide extends post-meal fullness. People find a single glass of water before meals, and logging portion sizes reduces nausea and makes meal planning easier; capturing those logs daily helps clinicians separate an actual side effect from normal early satiety during dose escalation.
3. Glucose-Dependent Insulin Secretion
Semaglutide enhances insulin release only when glucose is elevated, thereby improving glycemic control and reducing the risk of hypoglycemia. This mechanism is linked to better overall metabolic signaling, as trials show improved HbA1c outcomes, according to Infusion Health Telemedicine Clinic. Recording blood glucose trends alongside injections clarifies whether appetite shifts are medication-driven or glucose-driven.
4. Glucagon Suppression
By reducing inappropriate glucagon release from the pancreas, semaglutide prevents unnecessary hepatic glucose output, thereby decreasing hunger triggered by sudden glucose swings. Logging symptoms and timing relative to doses helps providers decide if titration adjustments or medication interactions are at play.
5. Energy Expenditure and Lipid Metabolism
Semaglutide increases energy expenditure and improves lipid handling, supporting fat loss and lean mass preservation when paired with protein and resistance training. Track activity, protein intake, and weekly body-composition trends to make small, evidence-based shifts that preserve muscle while fat comes off.
Centralizing the GLP-1 Patient Journey
Most people manage injections and symptom notes with calendars and scattered notes because they are familiar and low-effort. That approach works at first, but as doses change, meal timing, hydration, and side effects accumulate, data fragments across platforms and underlying patterns become obscured. Solutions like MeAgain centralize injection schedules, hydration, and protein targets, side-effect timelines, and trend visuals, turning scattered signals into coherent charts that clinicians and users can act on.
How Long Does Semaglutide Take to Work?
You can see early appetite shifts within the first month, but achieving a stable maintenance effect takes months as doses are titrated; typically, it takes about 17 weeks to reach final maintenance. Over longer trials, semaglutide produced significant, sustained weight reductions in many participants, consistent with findings reported by Infusion Health Telemedicine Clinic.
Patience matters:
The brain and body gradually relearn rhythms, and tracking dose timing, hunger ratings, and side effects during that window reveals whether progress is linear or requires clinician-guided adjustments.
Related Reading
• Liraglutide vs Semaglutide
• Semaglutide Belly Fat
• Compounded Semaglutide Side Effects
• Does Semaglutide Cause Hair Loss
• Semaglutide Weight Loss Side Effects
• Semaglutide Eye Side Effects
• How Long Does Compounded Semaglutide Last in the Fridge
• Who Should Not Take Semaglutide
• Semaglutide Visceral Fat
• Can Semaglutide Cause Depression
What Semaglutide Actually Changes Over Time (and What It Doesn’t)
Semaglutide often quiets the constant internal chatter about food. Portions feel more natural, and choices carry less emotional weight, but it does not eliminate the need for attention, structure, or support. You will likely notice fewer intrusive cravings and steadier intake, but stress patterns, eating-related habits, and the need for ongoing monitoring do not automatically change; this is normal biological adaptation, not failure. Lasting progress usually comes from combining that biological support with consistent routines and practical tools that translate physiology into daily actions.
Clinical Effectiveness and Research Results
The clinical evidence is ample and specific, and it tells us what to expect in real-world terms. In controlled programs that paired medication with lifestyle support, patients achieved substantial, measurable change: in a 68-week trial, participants taking semaglutide lost an average of 14.9% of their body weight, according to Advances in Therapy, reflecting the drug’s magnitude of effect when combined with structured behavior change.
What Those Numbers Mean Practically Is Straightforward
The medication shifts the odds in your favor, but the best outcomes in trials came when participants also used dietary and activity routines. That is why tracking dose timing, meal composition, hydration, and symptom timing matters; it aligns the drug’s pharmacology with real-life behavior, so clinicians and patients can see cause and effect rather than guessing.
Long-term Use and Weight Maintenance
Treat semaglutide as a chronic treatment that changes your physiological baseline while you use it, not a one-time cure. Stopping the medication commonly allows appetite signals to drift back toward pre-treatment patterns, so maintaining lost weight usually requires either continuing treatment or committing to durable lifestyle systems that compensate for the change in hormones.
This Pattern Appears Across Care Settings
People who cycle through diets experience emotional burnout and repeated regain. At the same time, those who pair sustained medication with clear, measurable routines tend to derive more benefit. The hidden cost of informal tracking is fragmentation, where dose times, side effects, water intake, and food quality are scattered across notes and memory, making it hard for clinicians to adjust titration or for patients to spot early trends. As complexity grows, outcomes slip.
From Manual Tracking to Clinical Clarity: Optimizing GLP-1 Outcomes
Most people manage this by manually writing notes or setting calendar alarms because it is familiar and low-friction. That works until titration changes, side effects, and meal timing diverge, at which point patterns hide and anxiety grows. Solutions like centralized GLP-1 app trackers aggregate injection schedules, hydration and protein goals, symptom timelines, and progress charts, providing clinicians with clear trendlines and users with a calm, actionable plan. In practice, that means fewer guesswork-driven medication changes and faster, evidence-based adjustments.
Lifestyle Integration and Clinical Tapering
Practical maintenance tactics you can act on now include prioritizing resistance training and protein intake to preserve lean mass, scheduling dose reminders that sync with planned meals, and keeping inflation-adjusted cost estimates for ongoing therapy in your financial plan so treatment surprises do not derail adherence. Clinicians often recommend gradual dose reductions rather than abrupt stops to blunt appetite rebound and minimize gastrointestinal symptoms. Careful logging during tapering helps determine whether regained hunger is transient or signals the need to resume a maintenance dose.
Debunking Common Myths
Myth
Semaglutide is only for people with severe obesity or diabetes.
Reality
Eligibility is broader than you think, and many adults with overweight and weight-related conditions qualify. The treatment is used across a range of metabolic profiles when clinicians judge the benefit-risk balance favorable.
Myth
Semaglutide removes the need for self-care.
Reality
The medication reduces baseline hunger and alters reward valuation, but it does not eliminate the need for mindful choices. You can still overconsume calorie-dense foods, and muscle loss is avoidable only when you combine medication with resistance work and adequate protein.
Myth
Facial changes are a drug side effect unique to semaglutide.
Reality
Facial volume loss follows rapid weight loss regardless of the method used, so changes attributed to the drug are actually a consequence of the speed and magnitude of the loss. Slower, managed reductions plus strength training reduce this effect.
Myth
Semaglutide is addictive.
Reality
There is no evidence of drug-seeking behavior or euphoria with semaglutide; the need to continue therapy reflects the chronic biology of weight regulation, not dependence.
Myth
It works fully on its own.
Reality
Optimal outcomes in trials paired the drug with structured lifestyle changes; the medication is a powerful aid, not a substitute for basic protective behaviors like adequate protein, hydration, sleep, and strength training.
A Concrete Comparison Helps
think of semaglutide as a supportive scaffold around a building under renovation. The scaffold reduces the risk of collapse and enables better work, but it does not replace the crew, materials, or schedule that deliver the final structure. Systems that map dose peaks to meals, log symptoms, and visualize week-to-week trends let you coordinate the scaffold with the work. One human pattern worth naming, drawn from care settings, is the stigma and secrecy that still surround GLP-1 treatment. When patients hide medication use or avoid asking for support, they miss early fixes for side effects and delay necessary titration changes. Normalizing transparent tracking and structured clinician feedback reduces shame and shortens the time to stable, comfortable dosing.
Centralizing Data to Reduce Diagnostic Latency
Most people manage injections and notes with scattered alarms and spreadsheets because that feels familiar. As doses change and side effects emerge, that approach fragments data, obscures context, and wastes clinicians' time. Platforms like GLP-1 tracking apps centralize injection schedules, hydration, and protein targets, side-effect timelines, and trend visuals, turning fragmented notes into actionable patterns and reducing the time clinicians need to determine whether hunger shifts are medication- or lifestyle-driven.
Transforming Clinical Insights into Patient Empowerment
That simple shift, from fragmented logs to a single, consistently updated picture, changes how clinical decisions get made and how people experience control. What happens next will expose who benefits most from support tools, and why the right system matters more than willpower alone.
Who Semaglutide is Typically Used for (and Why Support Tools Matter)

Semaglutide should be initiated and adjusted under medical supervision, and it is prescribed only after a clinician evaluates your full health context, as it alters hormonal signals and may interact with other conditions and medications. It is not a cosmetic shortcut; think of it as one medically supervised tool inside a broader plan that includes nutrition, activity, and monitoring. Support tools matter because motivation ebbs and the body adapts over time, so structure and timely feedback turn transient wins into lasting habits.
Who is Eligible for Semaglutide for Weight Loss?
In 2021, the Food and Drug Administration (FDA) approved the brand-name version of semaglutide, Wegovy, for chronic weight management in adults with obesity or overweight. The FDA specified that adults with an overweight and a weight-related health condition may qualify, including:
High blood pressure
Type 2 diabetes
High cholesterol
A licensed healthcare professional will assess your BMI, health history, medications, and readiness to follow a reduced-calorie diet and increased physical activity before prescribing Wegovy.
Why Must this Be Prescribed and Monitored?
The failure mode with self-directed use is avoidable and straightforward. Without baseline labs and medication review, side effects or interactions can be missed, and titration can become unsafe. When we supported patients through initiation, the pattern became clear in the first month. Clinical check-ins and symptom logs allowed clinicians to slow escalation rather than stop therapy, preserving continuity and reducing avoidable discontinuations. Clinicians also weigh benefits beyond weight, as long-term outcomes include cardiovascular effects. According to “The multifaceted impacts of semaglutide: exploring its broad therapeutic applications,” patients using semaglutide experience a 25% reduction in cardiovascular risk, which informs treatment decisions for many people.
How Do Support Tools Help When Motivation and Biology Shift?
Motivation is a waveform, not a constant. Biology adapts, and side effects often appear during titration windows, so a static calendar is fragile. Structured trackers let you align dose timing with meals and protein targets, distinguish normal early satiety from concerning nausea, and generate visual trends that a clinician can act on. Clinical evidence shows meaningful outcomes when medication pairs with behavioral routines. A study on the multifaceted effects of semaglutide reports that approximately 70% of patients using the medication achieved significant weight loss, underscoring the importance of careful monitoring and habit scaffolding to turn that potential into sustainable results.
Centralizing Patient Metrics for Faster Clinical Decisions
Most people rely on scattered alarms and notes because they are familiar and low effort. That approach works until dose dates, protein goals, hydration, and symptom logs multiply, hiding patterns and increasing anxiety. Platforms like MeAgain empathize with that reality, reveal the hidden costs of fragmentation by showing how missed context delays clinician decisions, and bridge the gap by centralizing injection schedules, hydration, protein targets, side-effect timelines, and trend visuals, so clinicians see signal rather than noise.
What About Stigma, Access, and Privacy Concerns?
This challenge appears across care settings: stigma around injectables and concerns about legitimacy lead some patients to hide use or chase unverified sources, which raises safety issues. When telehealth verification and documented symptom logs are available, patients gain confidence, clinicians get reliable data, and the risk of counterfeit exposure falls. Tools that create a secure record for your prescriber also reduce the shame that keeps people from seeking help, and that simple transparency speeds appropriate titration and side-effect management.
How Should You Reframe This Journey to Make It Feel Manageable?
Think of semaglutide as a precision instrument, not a magic wand; it tunes appetite and metabolism while you do the work of building muscle-sparing habits and consistent routines. Needing help does not mean something is wrong; it means you are using the right toolset. When people shift from private, anxious problem-solving to a visible, clinician-linked routine, they report less guilt and better adherence because the system supports them rather than requiring them to remember everything. That next piece exposes how design choices in a support tool actually change behavior in ways that feel more like relief than effort.
Related Reading
• How Much Protein Should I Eat on Semaglutide
• How Can I Track My Semaglutide Progress?
• How to Track My Semaglutide Side Effects?
• Semaglutide Body Composition
• Semaglutide Foods to Avoid
• What to Do When Semaglutide Stops Working
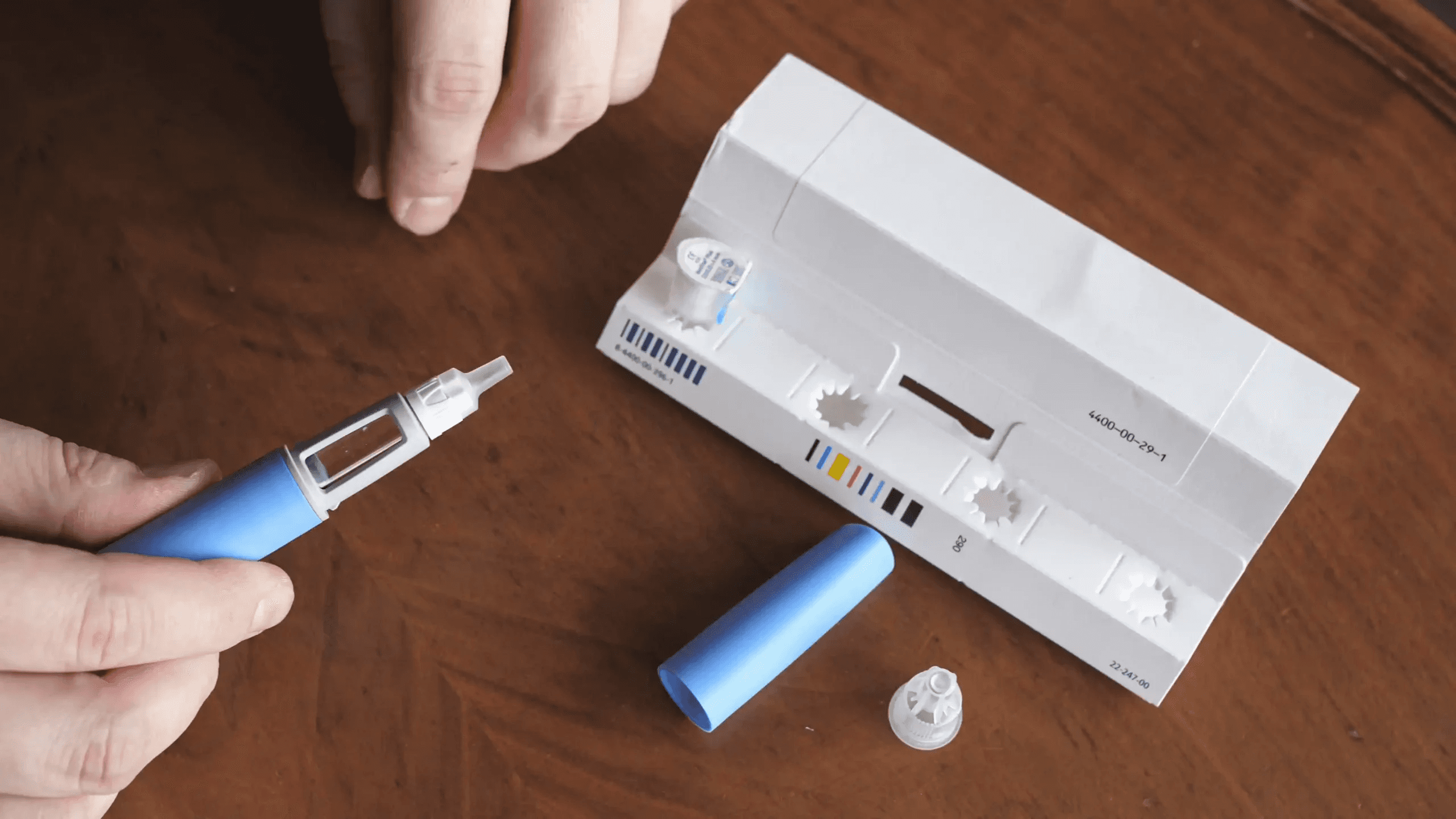
• How to Inject Semaglutide
• Semaglutide for Weight Loss in Non-Diabetics Dosage
• How to Track My Injections on Semaglutide?
• How to Track Food on Semaglutide
• Best App for Tracking Semaglutide Results
Download our GLP-1 app to Turn Your Weight Loss Journey into Your Favorite Game
Starting over is exhausting, and the loneliness of self-directed change turns daily habits into a grind that even a helpful drug cannot sustain. MeAgain acts as a companion, turning protein, fiber, water, and movement into a gentle game with an adorable capybara and a Journey Card that hands you steady feedback, momentum, and tiny wins like a pocket coach, so if you want kinder company while using Ozempic, Wegovy, or Mounjaro, consider trying MeAgain to make the day-to-day feel lighter.

