lifestyle
What is Compounded Semaglutide? Options, Safety, and Next Steps

You have read about semaglutide for weight loss or blood sugar control, and you see cheaper compounded versions offered by compounding pharmacies and online sellers. How does compounded semaglutide differ from brand-name prescriptions? Is the sterile preparation reliable? What about dosing, side effects, cost, and legal status? This article explains what compounded semaglutide is, its safety profile, standard dosing and injection options, and what to consider when choosing among local compounding pharmacies, telemedicine services, and FDA-approved products, so you can decide your next steps with confidence.
To help you sort through those choices, MeAgain's GLP 1 app lets you compare prescription and compounded options, connects you with licensed prescribers and vetted compounding pharmacies, and tracks dosing, side effects, and costs so you can move forward with confidence.
Table of Contents
Is Brand-Name Semaglutide the Only Option for Every Patient?
What is Compounded Semaglutide and How Does It Compare to Brand Names
Safety Considerations and Quality Standards for Using Compounded Semaglutide
Download Our GLP-1 Companion App to Support Safe Semaglutide Use
Summary
FDA currently approves three semaglutide products for specific uses, a narrow labeled pathway that, combined with insurer rules, creates frequent access barriers for many patients.
Real-world data show substantial clinical benefit: roughly 70% of patients report significant improvements in quality of life, and over 50% lose more than 5 kg within the first six months.
High patient demand reflects predictable results from approved products: more than 80% of brand-name semaglutide users report significant weight loss, which drives pressure to find alternative sources when access is blocked.
Cost motivates substitution, with compounded semaglutide sometimes priced up to 50% lower than brand-name formulations, a gap that matters when insurance denies coverage or prior authorization fails.
Quality and testing gaps are substantial across many compounded products. One analysis found that about 70% of compounded semaglutide prescriptions do not meet quality standards, and only 30% are tested for purity and potency.
Because compounded forms often require vial dosing, syringe draws, and variable formulations, consistent documentation and monitoring are essential to separate actual drug effects from supply or administration noise.
This is where MeAgain's GLP-1 app fits in: it centralizes dosing, side effects, and supply tracking, and connects patients with licensed prescribers and vetted compounding pharmacies.
Is Brand-Name Semaglutide the Only Option for Every Patient?
Many patients assume that brand-name semaglutide is the only legitimate or appropriate path for treatment. That belief oversimplifies how access actually works.
Coverage decisions, prescribing criteria, and supply constraints all influence whether a patient can obtain the drug, and these factors often push otherwise eligible patients toward alternatives or create frustrating therapy delays. Understanding these mechanics is critical because interruptions or delayed starts can undermine clinical benefits and patient confidence.
How Access Works in Practice
Insurance coverage is rarely automatic. Many insurers require specific diagnoses, such as type 2 diabetes or a BMI threshold, to cover brand-name products. Prior authorizations often include step therapy, detailed documentation, and, at times, repeated appeals.
Even when a patient meets clinical criteria, pharmacies may experience intermittent supply shortages, resulting in delays of days or weeks. Together, these barriers turn a seemingly simple prescription into a complex process, forcing patients to weigh cost, timing, and clinical priorities.
What is Semaglutide?
Semaglutide is a glucagon-like peptide-1 receptor agonist that mimics the gut hormone GLP-1. GLP-1 increases insulin release to lower blood sugar, slows gastric emptying to reduce post-meal glucose spikes, and promotes satiety, which helps curb appetite and lower caloric intake.
Which Brand Formulations Does the FDA Approve and What Do They Treat?
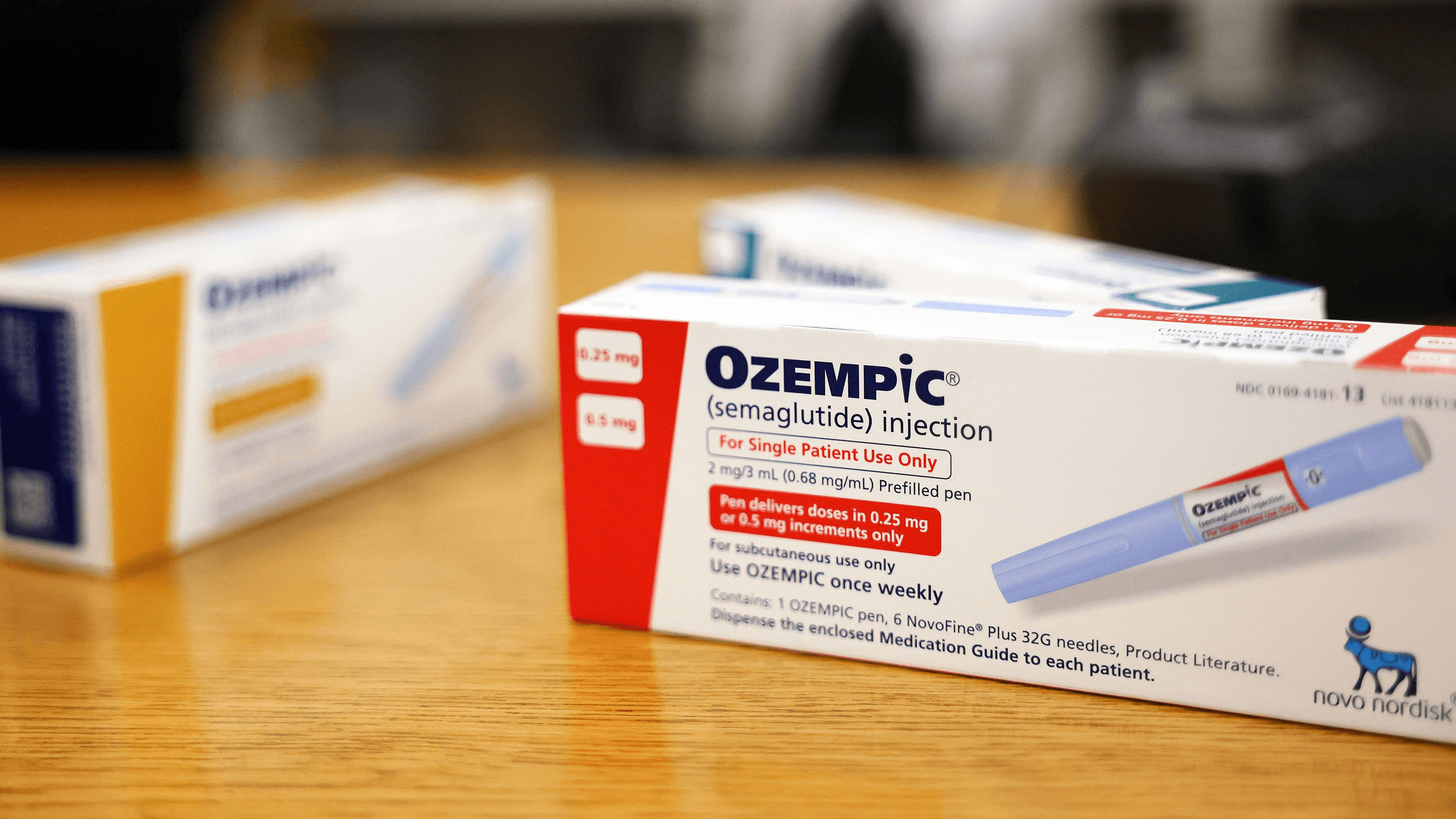
The FDA currently approves three semaglutide products with specific labeled uses: Rybelsus oral tablets and Ozempic injections for adults with type 2 diabetes who need better glycemic control, with Ozempic also lowering heart attack and stroke risk in patients with cardiovascular disease; and Wegovy injections for chronic weight management in adults and adolescents over 12 with weight-related health problems, used alongside diet and exercise.
Why Do Access Rules Make the Brand-Name Pathway Fragile?
This challenge appears across primary care clinics and specialty practices: insurers commonly tie coverage to a diabetes diagnosis or documented BMI thresholds, prior authorization processes require step therapy or detailed records, and pharmacies face intermittent supply issues. The result is delays or outright denials that force patients to stop, ration, or seek alternatives, and that bureaucratic stop‑start is exhausting and costly for people trying to maintain momentum in treatment.
How Effective is Semaglutide When Patients Can Actually Stay on It?
Real-world experience shows meaningful effects for many patients, as reported in Semaglutide in the Real World: Attitudes of the Population, where approximately 70% of patients reported a significant improvement in quality of life after switching to semaglutide.
One immediate clinical outcome clinicians monitor is weight change, and Semaglutide in the Real World: Attitudes of the Population reported that over 50% of patients experienced a weight reduction of more than 5 kg within the first 6 months of treatment.
Who Ends Up Exploring Compounded or Alternative Supplies, and Why?
After working through coverage appeals with patients over repeated denials, the pattern became clear:
People with PCOS, off-label weight concerns, or urgent metabolic risk often cannot meet insurers’ narrow criteria and face the choice of paying full retail for brand-name products, stopping therapy, or looking for compounded alternatives.
That pressure is more than inconvenience; it influences whether someone sustains a beneficial drug regimen or regresses because of cost and access barriers.
What are the Practical Risks of Switching Between Supply Sources?
Switching between brand-name and compounded or international supplies introduces variability in dispensing intervals, dosing records, and side-effect tracking, making it harder to assess effectiveness or attribute adverse events. It is exhausting when patients must cobble together calendars, text reminders, and spreadsheets to track injections and symptoms; that friction increases missed doses and undermines steady progress.
Solving the Complexity of Treatment Management
Most people manage that friction by juggling manual systems, but those habits break down fast as complexity grows. The familiar approach is using paper logs, phone alarms, and disconnected notes because it feels immediate and free. As dose changes, side-effect patterns, and refill timing pile up, errors creep in, missed doses become common, and anxiety spikes while clinical insight gets buried.
Platforms like MeAgain offer an alternative path. They centralize:
Shot reminders
Injection-site tracking
Hydration
Protein goals
In addition to simple logging, the schedule, symptoms, and nutrition are visible in one place, reducing dose errors and making side-effect patterns measurable rather than anecdotal. Clinicians and patients find that these features turn fragmented habits into reproducible data, reducing cognitive load and enabling treatment decisions to focus on outcomes rather than paperwork.
What Do Patients Feel When Access is Uncertain?
It is common to feel frustrated and anxious, especially when a successful course of therapy is interrupted by a denial or shortage. People describe scrambling to find alternatives, stocking extra vials when possible, or even exploring cross-border options out of desperation, all because the system treats medication access as negotiable rather than part of steady care. That emotional churn undermines confidence and makes treatment feel unstable.
What Should Patients and Clinicians Prioritize When Access is Limited?
If coverage is blocked, prioritize maintaining evidence-based dosing and documented monitoring over quick fixes that complicate later care. When alternatives are considered, insist on clear documentation of source, concentration, and lot information, and maintain consistent symptom and injection logs so clinical teams can separate actual drug effects from supply noise.
That gap between access and outcomes matters more than it looks, and the next section exposes the practical differences you need to weigh.
Related Reading
How Long Does Semaglutide Stay in Your System
What Is Compounded Semaglutide
Should I Take Semaglutide on an Empty Stomach
Does Semaglutide Cause Constipation
Why Does Semaglutide Cause Nausea
How Long Does It Take to See Results From Semaglutide
Does Semaglutide Make You Tired
Does Semaglutide Show Up in Blood Work
How Much Does Semaglutide Cost
How Does Semaglutide Work
What is Compounded Semaglutide and How Does It Compare to Brand Names

Compounded semaglutide is a pharmacist-made version of the active molecule semaglutide produced to meet a specific patient need, such as an alternate dose, a different delivery form, or an avoidance of a particular inactive ingredient. Compounding exists because licensed pharmacies can legally create tailored formulations when the commercially available, FDA-approved product does not meet an individual patient’s clinical requirements or when an approved product is temporarily unavailable.
Why Do Pharmacies Compound Semaglutide Now?
Pharmacies compound when the approved options do not match a patient’s clinical constraints, for example, an allergy to an excipient or a requirement for a dose not supplied by prefilled pens. This practice became more visible during supply squeezes, and it persists because some prescribers and patients want customization, different vial formats, smaller dose steps, or noninjectable forms.
The trade-off is straightforward: customization can address an access or tolerability issue, but it also introduces variability in formulation, sourcing, and handling that clinics must manage.
How is a Compounded Formula Actually Different From a Brand Product?
Think of brand-name semaglutide as a factory-made appliance, produced the same way every time, with tightly controlled components and rigorous testing. Compounded semaglutide is like a handcrafted version: the active drug may be the same base molecule, but inactive ingredients, the salt form used, concentration, and container type can differ.
Those differences matter for stability, absorption, and patient experience. For example, some compounded preparations use semaglutide salts rather than semaglutide base, a change regulators have warned can alter performance and safety.
Compounded semaglutide vs. Ozempic and Wegovy
What is the difference between compounded semaglutide and Ozempic, Wegovy, and Rybelsus? Their testing and approval, ingredients, and dosage forms are a few differences to consider.
Compounded Semaglutide | Ozempic and Wegovy | |
FDA approved? | No | Yes |
Where they’re made | Compounding pharmacies regulated by state boards of pharmacy or FDA-registered outsourcing facilities | FDA-registered Novo Nordisk facilities |
Ingredients | Inactive ingredients can vary; some pharmacies may use semaglutide salts or add extra ingredients | Contain semaglutide base; consistent ingredients used in each product |
Dosage forms |
|
|
Medication delivery (for injection) | Vials | Prefilled injection pens |
Dosage strengths | Varies |
|
Are the Nonstandard Dosage Forms Safe or Predictable?
No clinical evidence establishes the expected absorption or effect for many compounded forms, such as sublingual drops, oral disintegrating tablets, or nasal sprays. That uncertainty is not theoretical; it means you cannot reliably predict how much active drug reaches the bloodstream, how quickly side effects will appear, or whether the product will interact with other additives.
When a delivery form has not been studied in humans, the practical consequence is this: dosing becomes an experiment, and you notice that, in the way, side effects and benefits fluctuate across patients.
What Should You Worry About With Ingredients and Sources?
Quality risk comes in three flavors.
Altered chemical forms, such as semaglutide salts, may behave differently from the semaglutide base used in approved products.
Some suppliers sell material labeled only for research, not for human use, raising concerns about sterility and purity.
When pharmacies add vitamins or excipients to a compound, these additions may alter stability or cause unexpected reactions.
These are not hypothetical issues; they are the core reasons regulators caution against routinely substituting compounded versions when approved options are available.
How Do Dosing and Administration Practices Change With Compounded Products?
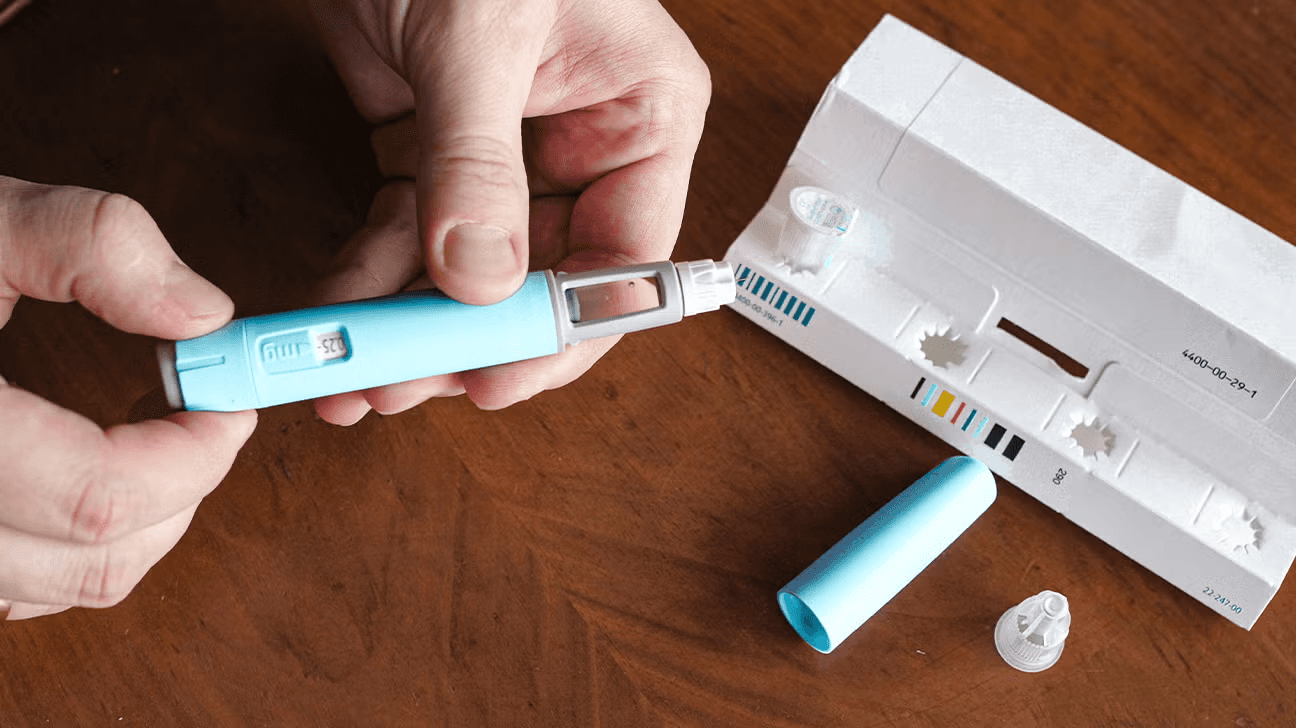
Compounded injections are commonly dispensed in vials rather than prefilled pens, so patients or caregivers must draw the exact doses with syringes. That adds steps where measurement error and contamination can occur.
Some compounding shops advertise microdosing, with tiny increments intended to reduce side effects. The problem is, microdoses have not shown the same efficacy in trials, so sticking to low, untested doses can slow or blunt the clinical progress people expect from standard regimens.
Will Cost Drive the Decision to Use Compounded Semaglutide?
Cost is a powerful driver in practice. According to InjectCo, compounded semaglutide can cost up to 50% less than brand-name versions, a difference that matters when insurance does not cover therapy or prior authorization fails. That price gap explains why some patients consider compounding, but cost savings do not erase the safety and evidence tradeoffs; choosing a cheaper product without verification of source, sterility, and potency shifts financial savings into clinical uncertainty.
How Do Patient Emotions and Clinical Patterns Show Up Here?
This challenge appears consistently across primary care and specialty settings: people want the personalization compounding promises, yet they feel anxious about quality and consistency.
The emotional pattern is clear:
Patients report relief when a tailored dose reduces allergy symptoms, but they also report renewed concern when side effects or benefits fluctuate.
Clinicians often view this as a two-step problem: the first is restoring access or tolerability, and the second is rebuilding reliable monitoring so that effectiveness and safety are not left to chance.
What Practical Steps Reduce the Risk if Compounding Is Considered?
If a clinician and patient decide compounding is necessary, insist on clear documentation of the drug source, lot numbers, and stability data, and require a monitoring plan that tracks side effects, weight, and injection timing. Use consistent logging so you can separate signal from noise, for example, monitoring injections, food intake, hydration, and symptoms on the same day each week. Those records make therapeutic decisions evidence-based rather than anecdotal.
Moving from Manual Friction to Integrated Clinical Monitoring
Most teams handle monitoring with paper notes or scattered messages because it is familiar and low-cost. That works at first, but as dose adjustments, refill timing, and side effects stack up, the scattered approach breaks down: records get lost, dose histories become inconsistent, and clinical judgment suffers.
Solutions like centralized GLP-1 tracking apps provide shot reminders, injection-site logging, hydration and protein goals, and simple symptom tracking, keeping a continuous, auditable record that enables clinicians to compare outcomes across formulations and dosing strategies without reconstructing the timeline from memory.
How Should Clinicians and Patients Think About Benefit Versus Evidence?
Demand for semaglutide is partly driven by strong outcomes with brand-name products, which has led to pressure to find alternatives. As noted by InjectCo, over 80% of patients using brand-name semaglutide report significant weight loss, underscoring patient interest in any available source.
That popularity creates a gap:
When approved, well-studied options deliver predictable results, but compounded alternatives lack the same evidence base. The honest stance is to treat compounding as a contingency or personalization tool, not as a substitute, without careful monitoring.
An Analogy That Helps Clinicians Explain Tradeoffs To Patients
Compounding is like commissioning a custom bicycle when a mass-produced model is out of stock or does not fit. The custom bike may fit your frame perfectly and feel better for certain rides, but unless the builder uses certified parts and tests the frame under load, you assume extra risk. You want a builder with documented parts, test records, and a warranty. The same caution applies to compounded medications.
That simple truth changes how you approach decisions about switching supplies, documenting doses, and tracking outcomes, and it’s why the conversation about safety and quality standards matters next.
That’s where the story gets more complicated, and the next section will expose why simple choices about sourcing and storage can have outsized consequences.
Related Reading
• Semaglutide Weight Loss Side Effects
• Compounded Semaglutide Side Effects
• How Long Does Compounded Semaglutide Last in the Fridge
• Liraglutide vs Semaglutide
• Does Semaglutide Cause Hair Loss
• Semaglutide Eye Side Effects
• Semaglutide Visceral Fat
• Semaglutide Belly Fat
• Who Should Not Take Semaglutide
• Can Semaglutide Cause Depression
Safety Considerations and Quality Standards for Using Compounded Semaglutide
Compounded semaglutide can be used safely, but only within a tightly controlled process:
Licensed pharmacies that follow sterile compounding standards.
Prescribers who document clinical necessity and monitoring.
Independent testing that verifies purity and potency.
If any of those pieces are missing, the risk of contamination, incorrect dosing, or unpredictable effects rises quickly.
What are the Risks of Semaglutide?
Risks fall into tiers you should watch and log carefully. Mild side effects commonly include:
abdominal pain
Heartburn
Belching
Nausea
Vomiting
Diarrhea
Constipation
More serious risks include hypoglycemia when semaglutide is used with other glucose-lowering drugs; watch for:
Rapid heartbeat
Shaking
Sweating
Dizziness
Nervousness
Irritability
Confusion
Immediate medical attention is warranted for:
Persistent upper abdominal pain radiating to the back
New skin rashes or hives
Swelling of the face or extremities
Breathing or swallowing trouble
Decreased urination
Vision changes
Headache
Slurred speech
Shakiness
Weakness
Mood changes
Drowsiness
Any sudden neurologic change
Why are Compounded Versions Riskier?
Compounded preparations add process risk, not a different pharmacology. They can become contaminated during compounding, contain excess active ingredient, or contain traces of unintended substances. Quality control failures are not rare, as noted by BodySpec Blog, “Approximately 70% of compounded semaglutide prescriptions do not meet quality standards.”
Independent verification is also uncommon; according to BodySpec Blog, “Only 30% of compounded semaglutide products are tested for purity and potency.” That means most compounded lots lack a third-party check you would expect for a high-risk injectable.
Under What Conditions Can Compounded Semaglutide Be Used Safely?
Use compounding only when every step in the chain is verifiable. Acceptable conditions include:
A state-licensed pharmacy prepares the product.
An FDA-registered 503B outsourcing facility with documented cGMP-like controls.
Sterile compounding follows USP 797 (sterile compounding) standards.
The active pharmaceutical ingredient is labeled for human use.
Each batch has a certificate of analysis and sterility/potency test results from an accredited lab.
The pharmacy keeps lot numbers and a traceable chain of custody.
Cold chain and storage conditions are documented.
The dispensing includes written dosing instructions, expiry dating, and pharmacist counseling.
Prescriber oversight must be explicit, with a written rationale for compounding, a monitoring plan, and scheduled follow-ups.
What Should Patients Verify Before Accepting a Compounded Product?
Ask for plain, specific proof.
Verify the pharmacy’s state license and whether it is an outsourcing facility registered under Section 503B.
Request a certificate of analysis and sterility test report for your lot, and confirm who performed the testing.
Confirm the API source, verify it is intended for human use, and ask how the product is stored and transported.
Get written dosing instructions and a clear plan from your prescriber that states how you will be monitored, what symptoms require urgent care, and when you will transition to an FDA-approved product.
Keep a physical or digital record of lot numbers and expiration dates, and retain the vial or packaging until you are confident no issues occurred.
Reducing Clinical Risk with Centralized Monitoring
Most people handle monitoring with phone alarms, sticky notes, or loose paper logs because those methods feel immediate and low-cost. That works until an adverse event or a supply switch forces clinicians to reconstruct dosing and timing from memory, delaying diagnosis and creating unnecessary risk.
Platforms like MeAgain centralize shot reminders, injection-site tracking, hydration and protein goals, and simple symptom logging, giving clinicians auditable timelines that make it easier to compare outcomes across formulations and reduce avoidable uncertainty.
How Should Prescribers and Pharmacies Coordinate Oversight?
Prescribers must document clinical need and write explicit transfer instructions when a compounded product is authorized, including exact concentration, volume per dose, syringe size if applicable, injection frequency, and emergency contacts. They should order baseline tests as indicated, set a schedule for symptom checks, and ensure MedWatch reporting is ready in case of adverse events.
Pharmacies must provide written batch records, testing certificates, and patient counseling at dispensing. Both parties should agree on a plan to transition to an FDA-approved product as soon as possible and record every encounter in the medical record.
What are the Immediate Steps If You Suspect Contamination or a Dosing Error?
Stop using the product and seek medical evaluation if you have worrying symptoms. Preserve the vial and packaging, photograph labels, and retain receipts. Ask the pharmacy for the lot’s certificate of analysis and sterility report.
If those are unavailable or inconsistent, report the event to your state pharmacy board and file an adverse event report with FDA MedWatch. Keep your prescriber informed and request a bridged supply that follows verified standards while clinical questions are resolved.
How Do Legal Changes Affect Current Users in Practical Terms?
Building on earlier guidance on FDA actions, clinicians should treat the regulatory phase-out as a trigger to prepare structured transitions, not as a cause for panic.
Practical measures include:
Documenting exact doses and dates for a smooth handoff.
Requesting short-overlap supplies to avoid missed doses.
Seeking prior authorization from the insurer based on the documented history.
Exploring manufacturer assistance or patient support for brand-name products.
Clinicians should also create a short-term monitoring checklist for patients to follow during the transition, so that new side effects are detected quickly and correctly attributed.
How Fragmented Tracking Jeopardizes Patient Safety
This is unsettling for patients because the choice is often between cost and certainty. After supporting clinics through several months of prior authorization and shortage cycles, the pattern became clear.
People feel desperate enough to accept uncertainty, and that anxiety makes consistent monitoring and documentation the most critical safety step.
What happens next is more consequential than most realize, and it will test whether your process protects you or leaves you scrambling for answers.
Download Our GLP-1 Companion App to Support Safe Semaglutide Use
Long-term semaglutide therapy requires consistent adherence, precise monitoring, and daily nutrition and hydration to support muscle function and digestion as you lose weight. We designed MeAgain to extend that safety plan into your daily routine, turning protein, fiber, water, and movement goals into a simple game with a capybara companion and a Journey Card so you stay organized, consistent, and informed whether you’re on brand or compounded semaglutide.
Related Reading
• Semaglutide Foods to Avoid
• Semaglutide for Weight Loss in Non-Diabetics Dosage
• How to Track Food on Semaglutide
• How to Inject Semaglutide
• How to Track My Semaglutide Side Effects?
• How Much Protein Should I Eat on Semaglutide
• What to Do When Semaglutide Stops Working
• How to Track My Injections on Semaglutide?
• Best App for Tracking Semaglutide Results
• Semaglutide Body Composition
• How Can I Track My Semaglutide Progress?

