lifestyle
How Long Does It Take to See Results From Semaglutide?

Losing weight can feel like a slow, frustrating journey. Even with diet and exercise, results often come in tiny, barely noticeable steps. That’s why many people turn to Semaglutide, a prescription medication clinically shown to support weight loss. But one question tops everyone’s mind: how long until I actually see results? Understanding the timeline helps set realistic expectations, track progress, and stay motivated without feeling discouraged. This article breaks down what research and real-world users reveal about weight loss with Semaglutide, from early changes in appetite to noticeable weight loss. It explains the factors that influence how quickly results appear.
To help you stay on track, MeAgain's GLP-1 app logs injections, weight, and symptoms, maps your personal timeline, and sends simple reminders so you can see when real, visible results from semaglutide typically begin and stay on track.
Summary
Semaglutide begins altering appetite quickly, with peak blood levels reached about one to three days after dosing, and many people notice reduced hunger within days.
Clinical trials and typical timelines show that measurable progress accumulates over months, for example, about 2 percent body weight loss by week 4, nearly 8 percent by week 16, and more than 34 pounds on average by week 68 in the Wegovy trial.
Stopping or interrupting therapy commonly triggers rebound, with one study finding that patients regained about two-thirds of the weight they had lost. Rebound often begins around eight weeks after discontinuation and continues for an average of 20 weeks.
Early adherence and routine matter, since consistent dosing and simple nutrition habits often produce 5- to 10-pound drops in weeks 4 to 8, while missed doses or start-stop patterns slow or fragment progress.
Behavioral supports amplify drug effects, specifically at least 150 minutes of moderate aerobic activity per week and protein targets of roughly 1.2 to 1.6 grams per kilogram of body weight to preserve lean mass (for example, about 136 grams daily for an 85-kilogram man).
Tracking simple metrics sharpens decision-making, for example, by logging five daily measures (dose taken and time, grams of protein, liters of water, plate balance or calories, and side effects) and using a three-week moving average to smooth out weight noise.
This is where MeAgain's GLP-1 app fits in: it centralizes injection reminders, protein and hydration logs, and side-effect tracking, enabling clinicians and users to link behavior patterns to outcomes.
How Long Does It Take to See Results From Semaglutide?

Semaglutide starts changing appetite almost immediately, but measurable weight loss is gradual: you often feel less hungry within days, then see steady pounds drop over weeks and months. Individual results depend on dose, how consistently you take it, and the diet, protein intake, hydration, and activity habits you maintain while taking the medication.
How Quickly Does Semaglutide Take Effect in the Body?
Semaglutide reaches peak concentration about one to three days after a dose, so its appetite-suppressing signals begin quickly. Early signals you might notice in the first days to weeks include a reduced appetite, feeling full sooner and for longer, fewer cravings, and a quieter internal “food noise.” Those sensation changes are the drug doing its job; actual scale changes usually follow once calorie intake and meal patterns settle.
What Did the Wegovy Trial Show?
A large 2021 Wegovy trial with almost 2,000 adults compared 2.4 mg semaglutide to placebo over 68 weeks while encouraging healthier eating and activity. Participants began losing weight within four weeks, with average losses of just over 2 percent by week 4 and nearly 8 percent by week 16, and an average of more than 34 pounds by week 68 on the active drug.
These trial results show that appetite shifts translate into progressive weight change when medication and behavior change go hand in hand.
Semaglutide Weight Loss Timeline
Week 4: About -2% of body weight
Week 8: About -4% of body weight
Week 12: About -6% of body weight
Week 20: About -10% of body weight, supported by findings from Doral Health & Wellness, including a 10% weight loss in 6 months, which reflects typical mid-phase outcomes.
1 year: About -15% of body weight, consistent with summaries such as Doral Health & Wellness: 15% weight loss in 1 year, 2025.
What to Expect Week by Week
Week 1–4, starting the journey: Hunger and cravings usually ease first. Many people don’t see big-scale changes yet, but the reduced urge to snack and smaller meal sizes create conditions for weight loss. Use this time to build simple habits you can sustain.
Week 4–8, gradual loss: Appetite suppression often produces 5 to 10 pound drops for many people, especially when meals become more protein-forward and hydration improves. Consistency matters more than perfection.
Week 8–16, more significant loss: As intake stays lower and activity nudges up, weekly losses become steadier and cumulative losses grow noticeably. Expect a more apparent change in how clothes fit and daily energy.
Week 16 and beyond, moving toward maintenance: Many people reach double-digit percentage losses by month 6 to 12, then shift focus to keeping those gains by holding steady behaviors and, if needed, adjusting dose under medical guidance.
Weekly Semaglutide Weight Loss Timeline
Week | Expected Weight Loss & Changes | Key Factors for Success |
Week 1 | Appetite suppression begins; minimal weight loss (~1-2 lbs). | Stay hydrated, eat balanced meals, and track food intake. |
Week 2 | Early weight loss of 1-5 lbs, mostly water weight; possible digestive adjustments. | Maintain consistent meal portions and avoid overeating. |
Week 3 | More noticeable appetite control; weight loss ~3-5 lbs total. | Continue portion control and focus on protein-rich foods. |
Week 4 | First significant progress; body adjusts to slower digestion. | Stick to a structured meal plan and stay physically active. |
Week 5-6 | Gradual fat loss begins; average 5-10% of initial body weight lost. | Incorporate regular physical activity (walking, strength training). |
Week 7-8 | Energy levels improve; consistent weight loss continues. | Maintain meal timing consistency and optimize hydration. |
Week 9-12 | Weight loss ~10-15% of initial body weight; improved metabolism. | Avoid processed foods and monitor long-term progress. |
Month 4-6 | Continued steady weight loss (~1-2 lbs per week); visible body composition changes. | Address plateaus with dietary adjustments and new exercise routines. |
Month 6-12 | Weight reduction reaches 15-20%+ of initial body weight; metabolism stabilizes. | Focus on long-term sustainability and lifestyle consistency. |
Beyond 12 Months | Weight stabilizes; maintaining new weight becomes key. | Develop lifelong healthy habits to prevent regain. |
Why Some People See Faster or Slower Results
Your biology and health profile shape responsiveness, including other medications or medical conditions.
Your dose matters because providers typically ramp up slowly to limit side effects; the therapeutic effects strengthen as the dose increases.
The form of semaglutide matters too; oral versus injectable differ in absorption and daily routine.
Missed doses delay steady-state levels and slow progress.
Lifestyle choices are not optional extras; they amplify the medication.
Adequate protein, consistent hydration, and timing of meals change the calories your body actually uses
What Patterns I See in Real Work With Patients
When we tracked people who logged daily injections, protein intake, and hydration, a clear pattern emerged. Those who maintained tight dosing and nutrition routines showed fewer plateaus by month four and reported less variability in appetite between doses.
Another recurring reality is the emotional mix of hope and frustration: many people want convenience, and when absorption or effect feels inconsistent, it often stems from variable dosing times or skipped injections. Insurance denials and high out-of-pocket costs also create a start-stop pattern that undermines long-term gains.
Why The Familiar Way Most People Manage This Creates Hidden Costs
Most people manage doses with notes on their phones or memory because it feels simple and low-friction. That familiarity works at first, but as life gets busy, those ad hoc methods let missed doses and untracked side effects accumulate, which fragments progress and increases anxiety about whether the medication is “working.”
How Platforms Like Meagain Change That
Platforms like MeAgain make those failure modes visible and actionable. By centralizing shot reminders, intelligent scheduling, protein and water tracking, injection-site logs, and side-effect notes, solutions like MeAgain reduce missed doses and provide a clear record of what actually happened, enabling clinicians and users to link behaviors to results and make targeted adjustments.
Common Misconceptions and Quick Corrective Advice
The truth is that semaglutide is not a fast fix on its own. Slow, steady progress is healthier and more durable than sudden drops, and the medication’s benefits compound when you pair it with consistent protein, hydration, and dosing routines. If appetite suppression feels inconsistent, focus first on dose timing and simple habit checks before assuming the drug has stopped working.
That success often masks a more challenging question: stopping too early, and the consequences are more surprising than most expect.
Related Reading
How Long Does It Take to See Results From Semaglutide
Should I Take Semaglutide on an Empty Stomach
Why Does Semaglutide Cause Nausea
What Happens When You Stop Semaglutide Too Early?
Stopping semaglutide too early usually means you stopped before the drug reached a stable therapeutic dose or before new eating and timing habits were firmly in place. The most common outcomes are a return of appetite, slowed or reversed progress, and absolute frustration that does not prove the medication failed.
Those effects occur because appetite-regulating signals and metabolic set points return to their prior state once the drug is removed. Hence, planning discontinuation with a provider matters as much as starting.
Why Does Stopping Right When You Hit a Goal Raise Risk?
Stopping semaglutide as soon as a goal is met is a good idea, but doing so too early can increase the chances of health problems returning. This can be discouraging and may make future treatment harder.
The body adjusts slowly, and discontinuing the medication should be planned carefully. Doctors usually suggest continuing therapy for a while after reaching a goal to help the body “lock in” the new weight or blood sugar level.
Is Ongoing Use Safer Than Abrupt Stopping?
In many cases, ongoing treatment is safer and more effective than stopping suddenly. Medical experts stress that reaching a target is not the end of care; it is part of a longer process of staying healthy and avoiding complications. Long-term follow-up and support are key parts of that process.
Who Should Decide When to Change Treatment?
Making changes to semaglutide treatment should always be done with a doctor's guidance, who can consider the whole picture of a person’s health. Reaching a goal is something to celebrate, but keeping those results takes just as much attention and care.
How Long Do Drugs Actually Hang Around, and Why Does That Matter Here?
To understand the effects of discontinuing semaglutide, let’s look at how long drugs stay in the body. Let’s also look at why some people choose to stop their medication. Most drugs will get out of your system quickly, but their side effects may stay for a while. In most cases, it doesn’t take long for the kidneys and liver to clear prescription drugs out of the body.
There will be traces of the drugs, but they are too small to have any significant effect. Meanwhile, those with liver or kidney disease will have large amounts in their system even after they’ve stopped taking it.
Why Do People Stop Taking Semaglutide Before They Should?
Some people may discontinue a medication after experiencing side effects, ranging from dizziness to heart palpitations. One of semaglutide’s most common side effects, for instance, is nausea.
The experience may be so uncomfortable that patients intentionally don’t tell their doctor that they’ve stopped the medication.
They might feel relief, but without the drug to manage an existing problem, symptoms could get worse.
In some cases, some may need to temporarily stop taking a particular drug due to a lack of physical capacity.
They may be unable to swallow, preventing them from taking oral medication. One of semaglutide’s brands, Rybelsus, used to treat type 2 diabetes, comes in tablet form.
What Does Withdrawal Look Like, and Can Tapering Help?
Withdrawal refers to the things someone experiences mentally and physically after stopping or reducing their intake of a specific medication. The higher the potential for dependency, the more severe and long-lasting the withdrawal symptoms can be.
Typically, people suffering from withdrawal will experience symptoms like changes in appetite and mood, irritability, nausea, tremors, or vomiting. To prevent withdrawal symptoms, your doctor may have you slowly reduce your intake of a drug, a process called tapering.
What Specifically Reverses When Semaglutide Stops Working?
Earlier, we discussed how semaglutide works to regulate blood sugar levels and curb appetite, promoting weight loss. In this section, we go into detail into how these effects are reversed when you stop taking semaglutide.
How Quickly Does Weight Come Back After Stopping?
Dr. Janice Jin Hwang, chief of the endocrinology and metabolism division at the University of North Carolina School of Medicine, says patients may notice effects of stopping semaglutide after a week or so. “Like any medication, when you stop taking it, it stops working,” adds Dr. Robert Gabbay, chief scientific and medical officer of the American Diabetes Association.
When discontinuing semaglutide, the process that regulates blood sugar levels and curbs appetite stops. Many, in fact, regain the weight they had lost. In a 2021 study, Dr. Domenica Rubino, director of the Washington Center for Weight Management & Research in Arlington, Virginia, found that people regained two-thirds of the weight they had lost.
This Pattern is Not Unique to Semaglutide
AOMs generally show a rebound after stopping, with weight regain beginning about eight weeks after discontinuation and continuing for an average of 20 weeks before plateauing, according to BMC (BioMed Central), meaning many people will see a steady rebound that unfolds over several months.
Similarly, trials of other powerful agents found that patients who completed a long course and then switched to a placebo regained a large portion of the weight they had lost, a result summarized in BMC (BioMed Central), underscoring that stopping a proven treatment often produces measurable backsliding rather than simple maintenance without support.
Why Do Hunger and Cravings Return Stronger?
Because of semaglutide’s delayed gastric emptying, people taking Ozempic, Wegovy, or Rybelsus feel fuller for longer. Once semaglutide is discontinued, however, feelings of hunger and cravings return.
Withdrawal symptoms can last from weeks to months as the body’s physiological baseline functions return to normal. “Without the medication, your gastric empty time will return to baseline which results in food being metabolized quicker and can be a trigger for you to feel hungrier faster or even requiring more food volumes to reach satiety,” adds Amy Lee, MD, Chief Medical Officer at Lindora Clinic in California.
What About Blood Sugar and Acute Medical Risks?
Discontinuing semaglutide may cause elevated blood sugar levels, leading to symptoms like blurred vision, fatigue, excessive thirst, and frequent urination. Some may even end up in the emergency room because of exhaustion and become more vulnerable to different infections.
“With the changes of active ingredient levels, you will likely feel the changes of the blood sugar as well, which can affect the way you feel about cravings and have effects on your overall appetite,” says Amy Lee, MD.
How Do Real People Feel When This Happens?
When we worked alongside clinicians tracking patients who stopped GLP-1 therapy, the pattern was consistent. Appetite spikes within weeks, weight often climbs back over the next two to five months, and motivation erodes as progress feels undone.
That emotional hit is severe; patients describe feeling discouraged, ashamed, or frightened that they must stay on medication forever, and that emotional energy often determines whether someone seeks medical guidance or simply quits on the plan.
Why The Usual, Familiar Approach to Stopping Fails, and What Can Change
Most patients manage medication changes through a scatter of notes, sporadic reminders, and memory. That approach is understandable because it is familiar and straightforward. Still, it creates hidden costs: missed doses, undocumented side effects, and no usable data for a clinician trying to taper safely.
Platforms like MeAgain address that friction by centralizing shot reminders, intelligent scheduling, protein and water tracking, injection-site and side-effect logs. Teams find this creates a clear record that clinicians can use to time tapering, spot early appetite rebound, and prescribe behavioral supports before rebound becomes a full backslide.
What About Supply Shortages and Forced Stopping?
While some patients stopped taking semaglutide due to unpleasant side effects, others had no choice given the shortage in supply. It’s an issue that will likely plague semaglutide manufacturer Novo Nordisk and its competitors for the long term. The Food and Drug Administration has listed Ozempic and Wegovy as “in shortage” for months.
Doctors may prescribe other medications, such as metformin or insulin, to help diabetic patients control their blood sugar. However, developing a new treatment plan can be challenging.
That supply-driven stopping shifts the decision from clinical planning to crisis management, raising the stakes for clear logs and routines that a new plan can quickly build on.
That frustrating rebound feels personal, but the reason it happens is primarily biological, and that means there are concrete, testable actions that can change the outcome.
Related Reading
• How Long Does Compounded Semaglutide Last in the Fridge
• Does Semaglutide Cause Hair Loss
• Who Should Not Take Semaglutide
• Semaglutide Belly Fat
• Compounded Semaglutide Side Effects
• Semaglutide Visceral Fat
• Liraglutide vs Semaglutide
• Semaglutide Weight Loss Side Effects
• Can Semaglutide Cause Depression
• Semaglutide Eye Side Effects
Tips for Optimizing Results with Semaglutide

You should expect to see the earliest appetite changes within days and measurable weight shifts within weeks. Still, the pace you actually experience depends on how steadily you dose and which daily habits you pair with the medication. Below are practical, concrete steps you can use right now to amplify semaglutide’s effects and protect your progress from predictable setbacks.
Follow your prescribed dosage: Gradual dosage increases help minimize side effects and improve long-term efficacy.
Keep The Timing Consistent
same day and in the same window each week, so blood levels remain predictable and side effects are easier to anticipate. Tying your injection to a fixed habit, such as brushing your teeth or drinking a morning coffee, significantly increases adherence.
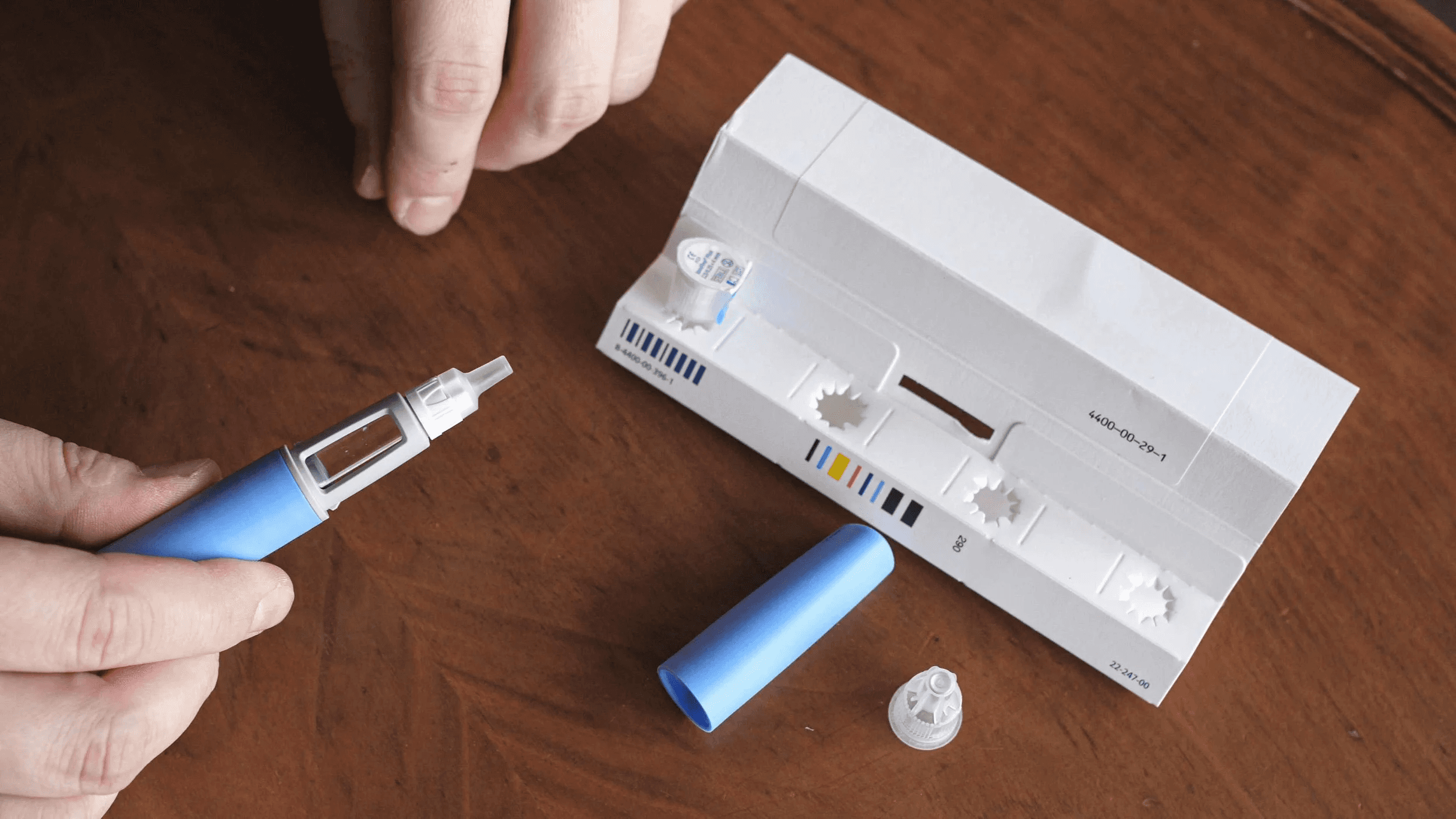
Prepare The Injection Properly
Store per label, let the pen reach room temperature before use, and rotate sites to reduce local reactions. Use a small log or a simple sticker on your calendar to record dose time and any acute side effects.
If nausea occurs early when doses increase, try small, bland pre-dose snacks, ginger candies, or spreading meals into smaller portions until the body adjusts. Then consult your clinician about slower titration rather than skipping doses.
When you miss a dose, follow your prescriber’s guidance. If you’re unsure, note it immediately so you and your clinician can correct the pattern before it costs weeks of progress.
Adopt a Balanced Diet
Focus on nutrient-dense foods like vegetables, lean proteins, and whole grains. Avoid processed foods, excess sugar, and unhealthy fats. A fiber-rich diet can help manage hunger, which Semaglutide can affect.
Because the drug lowers appetite, plan meals that deliver volume and nutrients without excess calories:
Half your plate should be vegetables
One quarter lean protein
One quarter whole grains
Starchy vegetables
Aim for 25 to 35 grams of fiber daily from whole foods, not supplements, to extend fullness between meals and to help with common side effects like constipation.
Evidence aligns with behavior change: reports show a 10% reduction in appetite, according to Oreate AI Blog, which you can use to shorten the window where hunger sabotages choices.
If family or cultural pressure centers meals on items that don’t fit your plan, try plate strategies. Smaller rice portions, shared dishes where you control your plate, or offering to cook one vegetable-forward option everyone can enjoy. These reduce social friction while preserving relationships.
Exercise Regularly
Aim for at least 150 minutes of moderate aerobic activity per week, along with strength training exercises to build muscle and boost metabolism.
Schedule three focused resistance sessions weekly that prioritize compound moves, for example:
Squats
Deadlifts
Presses
Rows
Using progressive overload across weeks. Strength work protects lean mass while calories fall.
For aerobic work, break 150 minutes into five 30-minute sessions or three 50-minute sessions, whichever fits your life; consistency matters more than a single long workout.
Track a simple training metric, like total weekly sets for major muscle groups or a measurable lift (e.g., squat), so you see strength improvements even if scale changes slow.
Stay Hydrated
Drinking enough water supports overall health and can help with appetite control.
Set a practical target, such as a reusable bottle marked by time, and aim for steady sipping rather than chugging; many people do well around two to three liters daily, depending on body size and climate.
Drink a glass of water 10 to 20 minutes before meals to blunt appetite peaks and reduce incidental snacking.
If you experience nausea or constipation, adding small amounts of electrolyte or mineral water can help without adding calories.
Track Progress
Keep a journal or use an app to track your food intake, exercise, and weight-loss progress. It can help you stay on track and make adjustments as needed.
Track five simple metrics daily or weekly: dose taken (yes/no and time), grams of protein, liters of water, total daily calories or plate balance, and a short note on side effects. That minimal dataset exposes patterns you can fix fast.
Use rolling averages for weight, for example, a three-week moving average, to avoid emotional reactions to day-to-day noise.
Capture non-scale wins: clothes fitting better, waist circumference, strength numbers, and mood scores, because they sustain motivation when the scale stalls.
Combining Semaglutide
For men with strength training and protein-rich meals can enhance weight loss while preserving muscle mass. Women may benefit from incorporating a mix of cardio exercises and nutrient-dense, fiber-rich foods to optimize results and support overall wellness.
For men focused on strength, target roughly 1.6 grams of protein per kilogram of body weight per day if you are doing progressive resistance training; for an 85-kilogram man, that is about 136 grams of protein daily, split across 3 to 5 meals with 20 to 40 grams per serving to maximize muscle protein synthesis.
Women often benefit from combining two to three strength sessions with regular cardiovascular exercise and aiming for 1.2 to 1.6 grams of protein per kilogram, with an emphasis on fiber-rich meals that stabilize energy and support reproductive and bone health.
Match training intensity and protein intake to your clinical context, and adjust based on strength logs and recovery. Preserving lean mass is critical for long-term metabolic health.
Sleep and Recovery
Reasonable rest accelerates gains and reduces appetite dysregulation.
Aim for 7 to 9 hours each night on a regular schedule; irregular sleep raises hunger hormones and undermines dietary discipline.
Build a Short Nighttime Routine
Dim the light
Turn off screens 60 minutes before bed
Avoid caffeine after 2 pm
Even small changes can improve sleep efficiency and reduce late-night calorie spikes.
Cost, Culture, and the Emotional Work
Practical ways to make the system sustainable.
Many people face the twin pressures of medication cost and social eating expectations, which create a start-stop pattern that kills momentum. If cost limits supply, maximize the value of every dose by tightening adherence, tracking side effects, and using predictable routines so no dose is wasted.
If social meals are unavoidable, plan micro-strategies: eat a small, high-protein snack before gatherings to reduce pressure, volunteer to bring a dish you can eat, and rehearse simple ways to say no to extra servings without fracturing relationships. These moves protect both progress and social ties.
Closing the Gap Between Intent and Consistency
Most people manage dosing and tracking in their heads or with notes because it feels familiar and straightforward, and that approach works early on but adds hidden costs as life gets busy. As schedules, stress, and travel increase, missed doses and fragmented logs accumulate, turning small slips into weeks of stalled progress.
Platforms like MeAgain provide automatic shot reminders, intelligent scheduling, protein and water trackers, and side-effect logs, giving users a single place to maintain consistent behavior and clinicians usable data to make targeted adjustments.
A Few Technical Tips That Make Daily Life Easier
Keep a week-ahead supply checklist and set a calendar alert to order refills, so supply interruptions do not cause an abrupt stop.
Use adjustable portion plates or pre-portioned containers to make balanced meals automatic on busy days.
When appetite declines during intense training, prioritize protein and quality calories post-workout to support recovery.
Semaglutide performs best when it is the steady prompt inside a broader routine you can live with long term, not a standalone shortcut; pair the medicine with predictable habits and you turn early appetite changes into lasting body composition shifts.
That next part is where everyday work becomes a sustainable system.
Download our GLP-1 app to Turn Your Weight Loss Journey into Your Favorite Game
When you start Ozempic, Wegovy, or Mounjaro, the medication does much of the heavy lifting, but protecting muscle and digestion requires daily attention. Consider MeAgain, which turns that attention into a game with an adorable capybara that nudges your protein, fiber, water, and movement targets.
Capture each milestone on a Journey Card and let the only all-in-one GLP-1 app make sticking with healthy habits feel as satisfying as the results.
Related Reading
• How Can I Track My Semaglutide Progress?
• How to Track My Injections on Semaglutide?
• Best App for Tracking Semaglutide Results
• How to Track My Semaglutide Side Effects?
• How Much Protein Should I Eat on Semaglutide
• How to Inject Semaglutide
• Semaglutide Foods to Avoid
• Semaglutide Body Composition
• Semaglutide for Weight Loss in Non-Diabetics Dosage
• How to Track Food on Semaglutide
• What to Do When Semaglutide Stops Working

