lifestyle
Why Does Semaglutide Cause Nausea? What’s Normal and What Helps?

The first week on semaglutide often starts with optimism. Appetite drops. Portions shrink. Then comes the nausea. Breakfast sits untouched. Coffee suddenly smells wrong. The question shifts quickly from “Is this working?” to “Is this normal?” Nausea is one of the most common side effects of semaglutide, especially during dose increases. For some, it’s mild and temporary. For others, it can feel disruptive enough to derail treatment altogether. This article explains why semaglutide can cause nausea, what symptoms are considered normal, when they signal a problem, and what helps reduce discomfort so weight-loss progress doesn’t come at the cost of feeling miserable.
MeAgain's GLP-1 app helps you track symptoms, identify patterns in food and timing that ease stomach upset, log dose changes, and receive reminders and practical tips to help you manage side effects and stay on treatment.
Summary
Nausea from semaglutide is a mechanism-based effect linked to slower gastric emptying and central satiety signaling, and it was observed in trials at 15.8% for Ozempic 0.5 mg, 20.3% for Ozempic 1 mg, about 20% for oral Rybelsus, and 44% for Wegovy 2.4 mg.
The symptom is strongly front-loaded and often improves, with a systematic review reporting nausea in 35% of patients during the first 4 weeks and falling to 20% after 12 weeks.
Patient variability aligns with procedural choices rather than mysterious intolerance, as trials reported a 44% incidence in the first 8 weeks with semaglutide 2.4 mg and 22% after 16 weeks, and real-world logs link rapid titration with irregular meals or low hydration to worse early episodes.
Simple behavioral changes have measurable effects: over 30% of patients report relief with smaller, more frequent meals, and dietary adjustments are cited to reduce nausea severity by about 40%. Ginger at doses near 1,500 mg per day is commonly recommended.
Structured tracking reveals predictable triggers: user logs over six weeks and analyses of the first 6 to 12 weeks show that dose timing, meal size, and hydration consistently correlate with nausea clusters and downstream adherence declines.
MeAgain's GLP-1 app addresses this by enabling users to log doses, meals, hydration, and symptoms, making patterns that predict early nausea during the first 4 to 12 weeks visible to users and clinicians.
Why Does Semaglutide Cause Nausea?
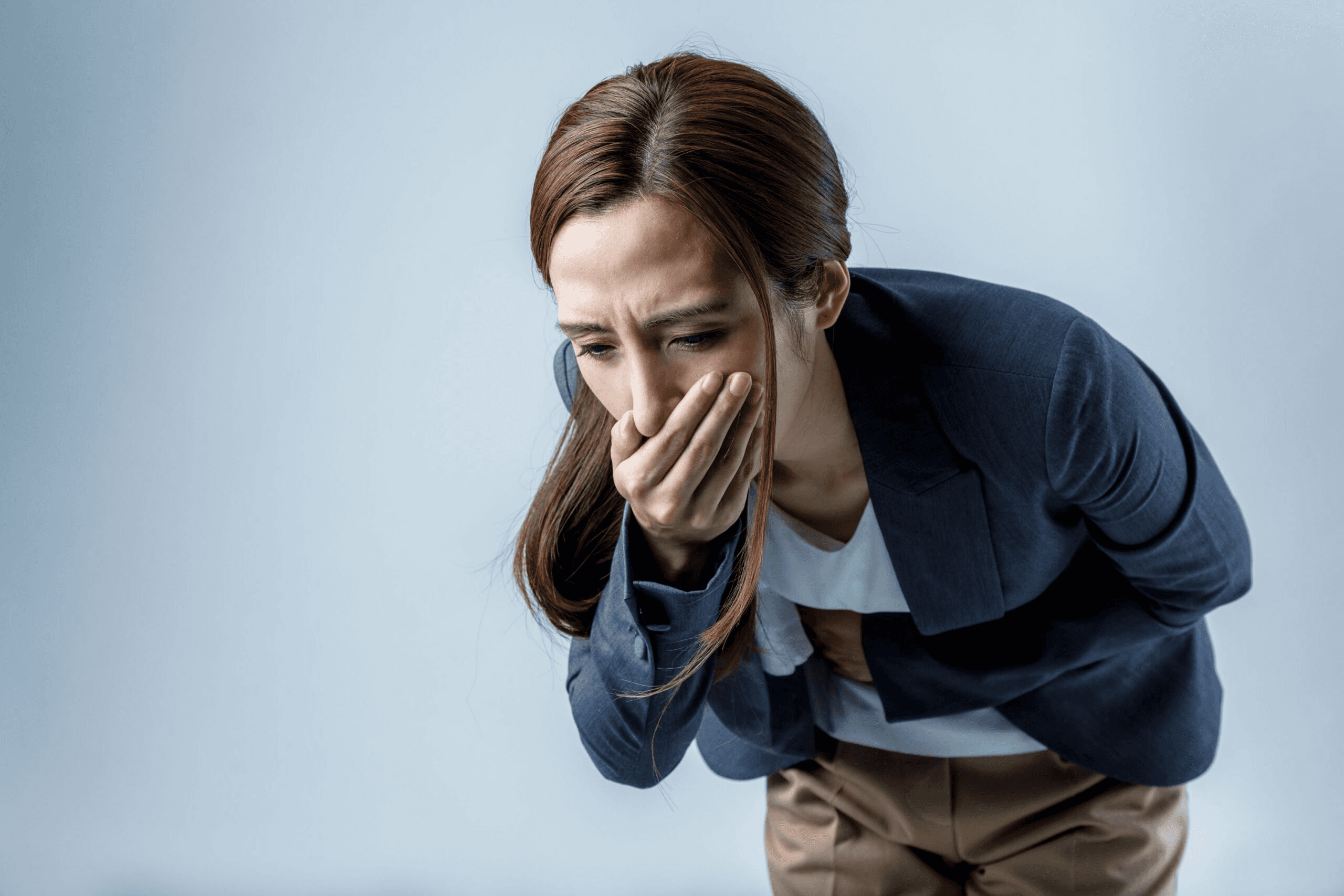
Yes. Nausea is not an accidental side effect of semaglutide.
It is a direct result of how the drug works in your body.
It slows gastric emptying and alters appetite signaling in the brain, which increases fullness and can trigger nausea, especially early in treatment and at higher doses.
In clinical trials, nausea increased with dose: Ozempic reported nausea in 15.8 percent of people on 0.5 mg and 20.3 percent on 1 mg; Wegovy (2.4 mg) had 44 percent reporting nausea; and the oral form Rybelsus recorded about 20 percent in trials.
Why Does Semaglutide Cause Nausea?
Semaglutide is a GLP-1 receptor agonist that works across the pancreas, gut, and brain. Activating those receptors delays the rate at which food leaves your stomach, so the stomach stays fuller longer. That slower emptying helps reduce appetite, but it also creates sensory signals your brain reads as bloating, pressure, or nausea.
GLP-1 signaling in the brain reduces “food noise” and reshapes reward and satiety circuits; animal models and human physiology suggest that the same central effects can cause nausea as a side effect. Think of it like narrowing an exit ramp on a highway: traffic slows, and the buildup produces discomfort.
Is Nausea a Sign The Medication is Intolerable or Failing?
Most people assume side effects equal failure. That’s the wrong assumption. Nausea is a predictable physiological response tied to the very mechanisms that make semaglutide effective.
The critical point is timing: a 2025 systematic review reported that nausea occurred in 35% of patients during the first 4 weeks of semaglutide treatment and decreased to 20% after 12 weeks. Those numbers match what we see in practice: early, dose-related discomfort that settles for many people as their bodies adapt.
What Patterns Actually Predict Who Will Struggle?
When we tracked users keeping structured side-effect logs through the first month of therapy, the pattern became clear: rapid titration and inconsistent meal or hydration habits correlated with worse early nausea.
The failure point is predictable, not mysterious. Push the dose too fast, leave intake patterns unchanged, and the body responds with stronger gastric signals. That’s why precise timing, gradual titration, and attention to what you eat around an injection matter more than vague “tolerance” talk.
From Guesswork to Clear Insights
Most people manage side effects by guessing and waiting; that approach is familiar and feels low-effort. Over time, that habit creates avoidable stops, starts, and anxiety people stop a helpful medicine because they never connected dose timing, meal size, and hydration to the nausea.
Platforms like MeAgain provide a different path: they let users schedule shots, log side effects in real time, and track protein and water intake so trends surface quickly. Teams find that with structured logging and simple reminders, users identify one or two modifiable triggers and reduce disruptive episodes, turning inconsistent guesswork into actionable, measurable adjustments.
When Should Nausea Trigger Urgent Concern?
For many people, nausea is mild and transient, but severe or persistent nausea can signal more serious issues. Seek emergency care if nausea is accompanied by persistent vomiting or diarrhea, severe abdominal pain that may radiate to your back, jaundice, fever, or clay-colored stool. These signs can indicate pancreatitis, gallbladder problems, or kidney injury and should be evaluated immediately.
Turning Symptom Fear into Smart Data
There’s a difference between an expected, dose-related queasiness that fades and a pattern that signals real danger; knowing which is which is what separates unnecessary fear from smart, data-driven decisions.
That insight feels like the end of the story until you realize that timing and personal patterns change how you manage it.
Related Reading
How Long Does It Take to See Results From Semaglutide
Should I Take Semaglutide on an Empty Stomach
Why Does Semaglutide Cause Nausea
When Semaglutide Nausea is Most Likely (and Why It Varies)

You should anchor nausea to timing and dose, not a personal flaw: it most often happens in the early weeks or right after a dose increase, and for many people it eases as the body adapts. That pattern is predictable, and the variability you feel usually comes down to how fast doses change and to everyday habits around food and fluids.
Why Do Experiences Vary So Much?
The same treatment can feel mild for one person and crushing for another because small procedural choices amplify the gut and brain response. Fast titration, for example:
Raises the intensity and frequency of symptoms.
Irregular meal timing or large, high-fat meals produce stronger gastric signals.
Low fluid or low-protein intake increases the risk of queasiness, which can lead to missed meals or skipped doses.
In trials of 2.4 mg semaglutide, 44% of participants reported nausea during the first 8 weeks of treatment, according to Gastrointestinal tolerability of once‐weekly semaglutide 2.4 mg in adults with overweight or obesity, which shows how common early nausea can be. That same study found the incidence of nausea decreased to 22% after 16 weeks of treatment, according to Gastrointestinal tolerability of once‐weekly semaglutide 2.4 mg in adults with overweight or obesity, and the relationship between gastrointestinal adverse events and weight loss, which makes clear the adjustment is tangible and measurable.
What Predicts Worse Episodes?
When we tracked side-effect logs across new users during the first 6 to 12 weeks, the pattern was consistent. Rapid dose increases, heavy meals soon after injections, and days with low water or protein intake were associated with clusters of nausea and fatigue.
That combination is exhausting; it undermines eating, saps energy, and pushes people to stop a treatment that otherwise helps them.
The emotional cost is real:
People feel anxious and helpless, and that uncertainty drives many to pause or quit.
Turning Guesswork Into Progress With Smarter Tracking
Most people handle symptoms by guessing and waiting, and that familiar method masks the actual cost, fragmenting adherence and quality of life. As a result, missed doses and inconsistent nutrition quietly accumulate, and users lose the momentum that makes therapy effective.
Solutions like MeAgain change that dynamic by letting users schedule shots, log side effects in real time, and track protein and water intake, so trends surface rather than being hidden; teams find that structured tracking turns guesswork into specific adjustments that reduce disruptive episodes while keeping privacy and simplicity intact.
How to Keep Control Without Overthinking It
Treat the early weeks like a tunable system, not a permanent verdict. Track dose changes, note what you ate and when, and log hydration and side effects so you can connect triggers to outcomes, then share those logs with your prescriber when adjustments are needed. That slight shift from intuition to recorded patterns makes nausea manageable and keeps you on track toward your health goals.
That sounds like progress, but the surprising part about managing it makes the next section essential reading.
Related Reading
• Can Semaglutide Cause Depression
• Semaglutide Eye Side Effects
• Does Semaglutide Cause Hair Loss
• Liraglutide vs Semaglutide
• Who Should Not Take Semaglutide
• How Long Does Compounded Semaglutide Last in the Fridge
• Semaglutide Visceral Fat
• Compounded Semaglutide Side Effects
• Semaglutide Belly Fat
• Semaglutide Weight Loss Side Effects
What Helps Reduce Semaglutide-Related Nausea?

Most semaglutide-related nausea gets better with time, and you can speed that process by matching what you do to how the drug works. Targeted, mechanism-aligned adjustments often reduce both the intensity and frequency of queasy episodes, helping you stay on treatment and in control.
How Do These Adjustments Actually Calm Nausea?
The gut and brain respond to physical volume and hormone signaling. Smaller meals and slower dose increases reduce mechanical stretch and blunt abrupt hormonal shifts, so the vagal and central signals that trigger nausea happen less often and with less force.
Avoiding heavy, high-fat meals reduces digestive workload and prevents strong CCK- and lipid-related responses that amplify queasiness. Steady hydration maintains blood volume and supports gut motility, helping prevent the cascade from tipping into persistent nausea.
Why Does Slower Dose Escalation Help?
When you gradually increase GLP-1 exposure, the nervous system has time to recalibrate appetite and satiety circuits without being overwhelmed by new signals. That calm adaptation matters because sudden increases create stronger visceral cues, which the brain interprets as nausea. In practice, staying on a lower dose for an extra month often reduces flare-ups enough that people continue therapy rather than stopping it.
What Role Do Meal Size and Composition Play?
Eating less at once reduces stomach load and shortens the window during which sensory receptors report fullness. Smaller, more frequent meals reduce peak gastric pressure and lessen the mismatch between slowed emptying and incoming food.
In fact, Healthline reported that over 30% of patients experienced nausea relief by eating smaller, more frequent meals, showing how a meal pattern alone can change symptoms within days to weeks.
A Practical Pattern We See
After tracking new users for six weeks using structured logs, the pattern became clear: people who avoided rich, fatty meals within two hours of dosing and kept small meals spaced throughout the day reported fewer and shorter nausea episodes. The failure mode was almost always the same: rapid titration, inconsistent eating, and low fluid intake, which turned manageable queasiness into a disruptive problem.
Most People Handle This By Guessing, and That is Where the Hidden Cost Appears
Most people follow informal rules: tough it out, skip a dose, or cut calories without clear feedback. That may seem low-effort at first, but it fragments adherence and hides the triggers.
Solutions like MeAgain change that dynamic. Platforms such as GLP-1 tracking apps let users schedule shots, log side effects in real time, and track protein and water intake, surfacing patterns so adjustments can be made before nausea forces a stop.
What You Should Expect, Not Promise
Mild to moderate nausea is not a sign of harm; it is a predictable response you can manage. Understanding the cause also lowers anxiety-driven sensations that make nausea feel worse. Patients who follow dietary adjustments experience a 40% reduction in nausea severity, according to Dramamine Blog, underscoring how practical changes can produce measurable relief.
Wegovy® or Ozempic®-Related nausea usually improves over time. But there are some things you can do to reduce your risk of nausea coming up and feel better if it does.
Here’s how to stop semaglutide nausea.
1. Follow Your Dose Escalation Plan
Your prescribing healthcare provider will start you on a low dose of semaglutide that gradually increases every month. This gives your body time to adjust, reducing the risk of side effects such as nausea.
If semaglutide nausea is severe, let your provider know. They recommend staying on your current dose longer before increasing it to give your body more time to adjust.
2. Eat Smaller, More Frequent Meals
Meals fill you up much more quickly while on semaglutide, and this fullness is uncomfortable.
Try eating smaller, more frequent meals throughout the day. This can help you get all the nutrients you need without overeating in one sitting.
Also, try tuning into your body and noticing when you start feeling full. Stop eating before you get overfull.
3. Avoid Foods and Drinks That Trigger Nausea
Certain foods and drinks can trigger nausea when taking semaglutide.
Try limiting or avoiding high-fat foods like:
Fatty meats
Baked goods
Greasy foods
Fried foods
These might also be triggering for some people taking semaglutide:
Spicy foods
Dairy products
Salty foods
Ultra-processed foods
Acidic foods like tomatoes or citrus fruits
Alcohol
Caffeine
Carbonated drinks
Strong smells
Monitor how your body reacts to these foods and drinks. Jotting things down in a food journal can help you spot patterns. If anything triggers nausea or any other gastrointestinal side effects, avoid it, especially while your body is still adjusting to the drug.
The good news is that if you’re taking Ozempic® or Wegovy® for weight loss, limiting high-fat and processed foods can help you reach your weight-loss goals and reduce nausea.
4. Eat Foods That Soothe (or Don’t Worsen) NauseA
Go for bland, easy-to-digest foods when you’re really feeling nauseous, such as:
Chicken
Fish
Potatoes
Rice
Plain toast
Bananas
You can also try eating these nausea-soothing foods 30 minutes after taking semaglutide:
Apples
Mint
Plain crackers
Ginger-based drinks
5. Try ginger
Speaking of ginger, it may just be one of the best things you can eat when you’re feeling nauseated. Ginger has been studied for its anti-nausea properties across a range of conditions, from pregnancy to chemotherapy. To relieve nausea from semaglutide, you can try a ginger chew or sip ginger tea.
You may want to avoid ginger ale, however, as the carbonation may worsen nausea (plus, some ginger-based sodas may contain a lot of sugar)
You can even take a ginger supplement in a gummy, powder, or capsule form.
Some research suggests that taking 1,500 mg of ginger per day, divided into doses (e.g., two to three times per day), can relieve nausea. When adding a new supplement to your routine, it’s a good idea to check in with your healthcare provider to make sure it won’t interact with any medications you’re taking.
6. Drink Plenty of Water
Stay on top of your hydration. Instead of gulping down large amounts of water at once, take small sips throughout the day. That said, avoid water 30 to 60 minutes before and after meals and during meals to see if that helps reduce nausea. The idea is that it leaves more room in your stomach for food.
In addition to helping with nausea, drinking water can help regulate your appetite, relieve constipation, and replenish lost fluids if you experience vomiting or diarrhea related to semaglutide.
7. Limit Activity After Meals
Avoid vigorous activity right after meals. Schedule exercise earlier or later in the day, away from meal times.
On the flip side, avoid lying down when you’re feeling nauseous, as this can make you feel worse. After you’ve eaten, or when nausea hits, sit comfortably or go for a gentle walk.
8. Do Something Distracting
Do an enjoyable or distracting activity to take your mind off your semaglutide side effects until they pass. If you’re not feeling up for much, try sitting comfortably and watching TV, listening to a podcast, or reading a book.
9. Try Anti-Nausea Medications
Anti-nausea medications can help reduce how sick you feel on semaglutide. You can get over-the-counter anti-nausea drugs or supplements, such as:
Bismuth subsalicylate (Pepto-Bismol®)
Dimenhydrinate (Dramamine®)
Ginger
You can also ask your healthcare provider about prescription anti-nausea medications, such as ondansetron (Zofran®).
Zofran is approved by the Food and Drug Administration (FDA) to reduce nausea and vomiting caused by radiation, surgery, and chemotherapy. Medical providers often prescribe it for other types of nausea, too. You can take ondansetron as needed when nausea crops up. It should start working within an hour, sometimes sooner.
10. Speak to Your Healthcare Provider
Don’t be afraid to reach out to your prescribing healthcare provider if semaglutide nausea is hard to deal with. There are several things they might consider doing to help, including lowering your dose or keeping you on your current dose for longer.
Your provider may also prescribe anti-nausea medication or recommend other nausea remedies not listed here.
11. Consider Semaglutide Alternatives
If semaglutide nausea really doesn’t get better, your healthcare provider may recommend a different medication for weight loss or weight management.
Semaglutide alternatives could include:
Tirzepatide (Mounjaro®, Zepbound®)
Liraglutide (Victoza®, Saxenda®)
Metformin
Topiramate
Some of these medications are FDA-approved to help people with type 2 diabetes manage their blood sugar levels. But a healthcare professional may prescribe them off-label for weight loss.
Others are FDA-approved for obesity or overweight if you have a weight-related medical condition. A healthcare provider can help you decide on the best medication for you.
12. Adjust your eating habits
Starting semaglutide often requires significant changes, including weekly injections, a new exercise routine, and a new diet. Semaglutide changes how quickly your body digests food, so you may not be able to eat as much as you used to. The way you eat can make a big difference in how comfortable you feel while taking semaglutide.
Here are some ways to adjust your eating habits for more success and less nausea on semaglutide:
Only eat when you’re hungry, and stop eating once you feel full. It may sound obvious, but hear us out. Because semaglutide slows down digestion, you’ll have to rely more on how you feel vs. how much food is left on your plate to know when you’re full.
Practice Mindful Eating
Mindful eating focuses on eating without distractions, paying attention to how the food feels and tastes in your mouth. Being more mindful can help you start to recognize when you’re full and when you’re really hungry. It can also help you avoid overeating and get more satisfaction from your food.
Eat Smaller Meals, More Often
For people taking semaglutide, experts often recommend eating smaller meals more often rather than larger meals less frequently. Like mindful eating, this can help you gain better awareness of your hunger and fullness cues. It also reduces the likelihood of overeating and inducing nausea.
That simple change in routine can shift weeks of uncertainty into predictable progress. Keep reading, because the next piece shows how to turn those routines into a habit you actually enjoy.
Related Reading
• How to Track My Semaglutide Side Effects?
• Semaglutide Body Composition
• How to Track Food on Semaglutide
• Semaglutide for Weight Loss in Non-Diabetics Dosage
• How Much Protein Should I Eat on Semaglutide
• Best App for Tracking Semaglutide Results
• How Can I Track My Semaglutide Progress?
• Semaglutide Foods to Avoid
• How to Inject Semaglutide
• What to Do When Semaglutide Stops Working
• How to Track My Injections on Semaglutide?
Download our GLP-1 app to Turn Your Weight Loss Journey into Your Favorite Game
You’ve seen how semaglutide side effects follow predictable patterns, and managing them alone can turn small daily choices into lost momentum. MeAgain turns that work into a game with an adorable capybara that nudges you toward the right micro-habits and a Journey Card that captures every milestone, so progress stays visible and motivating.
Download MeAgain and turn your weight loss journey into your favorite game.

