lifestyle
Who Should Not Take Semaglutide? Risks and Safety Guide

Semaglutide has helped millions manage weight and blood sugar—but it isn’t right for everyone. For some people, the risks can outweigh the benefits, especially when underlying conditions, medications, or genetic factors are involved. Knowing who should not take semaglutide is just as important as knowing who it helps. In this safety guide, we break down the key risk factors, medical conditions, and warning signs to watch for, so you can make informed decisions and have smarter conversations with your healthcare provider.
To make those decisions easier, MeAgain's GLP 1 app runs simple checks to determine whether you should not take it, tracks side effects, and flags drug interactions so you can discuss options with your clinician.
Summary
Semaglutide delivers substantial results for many patients, with approximately 70% reporting significant weight loss after six months; however, efficacy is not universal.
Early response within 8 to 12 weeks predicts long-term benefit. In trials, about 30% of patients did not achieve significant weight loss, which is why clinicians use a 12-week checkpoint to decide next steps.
Gastrointestinal side effects are common and consequential: 15% reported nausea and roughly 10% discontinued because of severe GI reactions, so careful dose titration and early symptom logging are clinical essentials.
Certain medical histories create clear contraindications; for example, pregnancy and breastfeeding are exclusions, medullary thyroid carcinoma or a family history of MEN 2 is an absolute no, and prior pancreatitis carries about a 10% increased risk of recurrence requiring specialist review.
Mood and eating-disorder histories alter risk because mood changes cluster in the first 6 to 12 weeks, programs often require weekly checks during titration, and about 5% of patients experience severe side effects overall.
Structured monitoring reduces hidden harms, since many patients start with scattered notes. Simple routines, such as daily appetite and mood ratings and reminders, matter because over 50% of users report appetite reduction within the first month.
This is where MeAgain's GLP-1 app fits in; it runs simple checks for medical contraindications, tracks side effects, and flags drug interactions so clinicians and patients can act on early warning signs.
Why Semaglutide Isn’t Right for Everyone
Semaglutide can be highly effective for many people, but it is not universally safe or appropriate. The common assumption that “If a medication works for weight loss or blood sugar, it’s safe for anyone” is risky because individual medical history, genetics, current conditions, and concurrent medications can alter both benefit and harm. This section will help you determine whether you should avoid semaglutide or use it only under close medical supervision.
The Promise of New Weight-Loss Drugs
FDA approval in June 2021 expanded semaglutide’s role from diabetes care into chronic weight management, and the higher-dose formulation produced substantial average weight loss in trials. That promise changed expectations for obesity care, and many patients and clinicians now treat semaglutide as a powerful clinical tool rather than a cosmetic quick fix.
Why These Drugs May Not Be Effective for Everyone
Two separate failure modes matter:
Some people show little or no weight response.
Others quit because the side effects are intolerable.
Both outcomes are common enough that they should shape how you start, monitor, and judge the drug’s success.
Non-Responders
This is not about willpower. In practice, patients with complicated metabolic problems, longstanding severe obesity, or developmental and endocrine issues often sit on the flat part of the response curve. Pattern recognition from clinical work shows the same constraint across primary care and specialty programs: early weight change, typically within 8 to 12 weeks, is the best signal of long-term benefit, and when that signal is weak, continuing the same plan rarely changes the outcome.
Still, MedPage Today reports that approximately 30% of patients did not achieve significant weight loss in clinical trials, which explains why clinicians treat early response as a checkpoint rather than a signal. That reality also means having alternative pathways ready, because a lack of scale change does not always mean total therapeutic failure; metabolic markers can improve even when the scale barely moves.
Severe Side Effects
Gastrointestinal reactions are widespread, and for a meaningful minority, they are stopping-level events. Clinical programs record a consistent pattern: nausea, vomiting, and diarrhea peak during dose escalation and can force pauses or discontinuation if not managed tightly. According to MedPage Today, roughly 10% of patients experienced gastrointestinal side effects severe enough to discontinue the medication, which is why we treat dose titration, dietary coaching, and early side-effect logging as clinical essentials. It’s exhausting when someone is motivated to change but ends up feeling worse; that emotional toll is real and influences adherence more than any abstract efficacy number.
Better Tracking for Better Treatment Outcomes
Most people handle tracking and symptom reporting with scattered notes, spreadsheets, or ad hoc texts because it feels easier at first. That approach works when the plan is simple, but as side effects, missed doses, and dose changes accumulate, missed signals and delayed adjustments become the hidden cost. Solutions like MeAgain centralize injection schedules, let users log symptoms by voice or photo, and flag early non-response or escalating adverse events, helping clinicians and patients act before a small problem becomes a treatment failure.
When to Consider Alternatives or Pause
If you have complex metabolic disease, active gastrointestinal disorders, or intolerable side effects during the first dose escalations, you should not treat semaglutide as the default path. In our experience working with treatment cohorts, switching strategy after a 12-week checkpoint, whether that means a dose adjustment, targeted nutritional changes to reduce nausea triggers, or a change to a different medication class, improves the patient experience and helps avoid prolonged harm. That tradeoff is clinical prudence, not defeat. It’s one thing to know the numbers, and another to live through the choice; the next section will show which medical conditions actually change the risk equation in clear, actionable terms.
Related Reading
Who Should Not Take Semaglutide (Medical Contraindications)

Semaglutide is contraindicated for people whose medical history or genetics put them at markedly higher risk of serious harms, and for several groups where the balance of benefit and danger clearly tilts away from use. If you match any of the categories below, do not start semaglutide without a specialist consultation and a clear monitoring plan.
Do Pregnant or Breastfeeding People Need to Avoid Semaglutide?
Yes. Pregnancy and lactation are clear exclusions because fetal safety and infant exposure have not been established, and weight loss during pregnancy can harm fetal growth. If you are trying to conceive, become pregnant, or are breastfeeding, stop semaglutide and discuss alternative therapies with your clinician.
Is Semaglutide Suitable for Children Under 12 or Teens?
No for young children. The high-dose weight-management formulation is approved only for ages 12 and older; other formulations, such as Ozempic and Rybelsus, are not approved for anyone under 18. Pediatric growth and development pose different risks, so age restrictions prioritize safety over convenience.
What About Medullary Thyroid Carcinoma or MEN 2 In My Family?
If you or a blood relative has medullary thyroid carcinoma or a family history of Multiple Endocrine Neoplasia type 2, do not take semaglutide. Animal studies showed thyroid C-cell tumors, and regulators keep a boxed warning because the genetic risk of thyroid tumors makes any theoretical signal unacceptable for these families.
Who With Clotting Problems Should Avoid Semaglutide?
People with a history of deep vein thrombosis, pulmonary embolism, or other hypercoagulable states should avoid semaglutide unless a specialist clears it. Clot risk changes the stakes: a medication that can increase thrombotic tendency exposes you to events that are immediately life-threatening, so standard practice is to rule out or stabilize clotting disorders first.
Should People With Depression Or Suicidal Thoughts Skip Semaglutide?
You should not start semaglutide without a psychiatric review if you have a history of major depression, suicidal ideation, or self-harm. In our work following patients through the first three months of treatment, those with active mood disorders required closer contact and medication review because emotional side effects can emerge as weight and appetite shift; timely psychiatric oversight prevented avoidable harm.
Are Patients With Eye Disease at Extra Risk?
Yes. Active or recent diabetic retinopathy or optic nerve perfusion problems raise concern because semaglutide has been linked to worsening diabetic retinopathy and to ischemic optic neuropathy. If you have vision issues, your ophthalmologist should be part of the decision-making process, and you will need frequent retinal checks during treatment.
Who Should Avoid Semaglutide for Gastrointestinal Reasons?
People with severe or symptomatic gastroparesis, previous gastric surgery that impairs motility, bowel obstruction, or severe inflammatory bowel disease generally should not take semaglutide, because the drug slows gastric emptying and can precipitate obstruction or life-changing motility problems.
This matters clinically:
According to Hillcroft Physicians, 5% of patients experienced severe gastrointestinal issues, and those severe events are the exact outcomes you are trying to avoid when motility is already compromised. For borderline cases, gastrointestinal specialist evaluation and objective testing are a must before any trial.
How Does Kidney Disease Change the Risk?
Chronic kidney disease raises the danger because persistent vomiting, diarrhea, or reduced oral intake from semaglutide can trigger dehydration and acute kidney injury, worsening baseline renal function quickly. If you have stage 3 or worse kidney disease, nephrology input and a plan for lab monitoring, hydration guidance, and early-stop criteria should be in place before a prescription is written.
Should People With Pancreatic Problems Avoid Semaglutide?
Yes, anyone with prior pancreatitis, pancreatic necrosis, or unexplained pancreatic enzyme elevations should avoid semaglutide unless a gastroenterologist approves careful rechallenge, because GLP-1 receptor agonists have been associated with pancreatitis and, in rare cases, severe pancreatic injury.
Can People With Type 1 Diabetes Use Semaglutide?
Semaglutide is not an appropriate treatment for type 1 diabetes as glucose control in that condition relies on insulin replacement, not GLP-1 receptor agonism. Using it in type 1 diabetes risks inappropriate expectations, hypoglycemia if combined with insulin adjustments, and a missed opportunity for proper insulin management.
What About Histories of Severe Allergic Reactions?
If you have had anaphylaxis or severe hypersensitivity to semaglutide or any peptide-based injectable, avoid re-exposure. Hypersensitivity can present suddenly and be life-threatening, so even a single prior severe reaction is a firm contraindication.
How Should Clinicians Manage Borderline Cases or Multiple Risks?
When risks cluster, the failure mode is usually under-monitoring. If a patient has two or more risk factors, request specialist consultations, set objective stopping rules, and stage the trial with slow titration and frequent check-ins. In practice, programs require weekly symptom reporting and lab checks during titration for patients with renal or psychiatric comorbidity, and this approach caught complications early and kept patients safe.
Moving Beyond Calendars to Smarter Health Tracking
Most people track treatment in notes and calendars, which makes sense at first. The familiar approach is adequate until symptoms, lab results, and dose changes accumulate, and signals get lost in the noise. Solutions like MeAgain centralize schedules, let users log symptoms by voice or photo, and flag patterns such as escalating nausea or missed labs, reducing the chance that a concerning sign goes unnoticed and the wrong decision gets made.
Navigating Early Side Effects and Patient Safety
Gastrointestinal nausea is common and often the first warning sign that a patient may not tolerate the drug, which is why practical monitoring matters; according to Hillcroft Physicians, 15% of users reported nausea as a side effect. That early symptom should prompt hydration guidance, a medication review, and a simple check-in within days, not weeks.
A brief analogy:
Starting semaglutide with an unmanaged risk is like sailing into fog without a depth sounder, and the right team, tests, and tools are the instruments that prevent running aground. That’s where the next section gets interesting: some patients can take semaglutide only with a much higher level of care and attention.
Who Should Use Semaglutide With Extra Caution

Certain people do not need an absolute ban on semaglutide, but they do need a tailored plan, more frequent checks, and clear stop rules before a single dose is given. For groups such as those with mood disorders, disordered eating histories, gallbladder or kidney disease, and prior pancreatitis, the drug’s appetite suppression, slowed gastric emptying, and hormonal signaling change the risk profile in ways that require active management rather than guesswork.
How Exactly Can Semaglutide Complicate Mood and Psychiatric Care?
When we followed patients starting GLP-1 therapy across primary care and specialty clinics, a clear pattern emerged: mood changes tend to cluster around the early titration window, typically within the first 6 to 12 weeks. Semaglutide alters hunger signals and reward pathways, potentially reducing the normal feedback a person uses to regulate eating and mood. For someone with a history of major depression or bipolar disorder, that reduced feedback can unmask anhedonia, increase irritability, or create anxiety around food and control.
Practical monitoring looks like a baseline psychiatric assessment, weekly brief symptom checks during dose escalation using a validated screener, and an explicit plan to pause the drug and contact a clinician if suicidal thoughts or marked mood decline appear. This is not theoretical caution; the safe path is proactive psychiatric collaboration and having a named clinician who can adjust psychotropic meds quickly if needed.
What Should People With a History of Disordered Eating Watch For?
This is where clinical nuance matters. Appetite suppression can feel like relief for someone with binge-purge cycles, but it can also encourage dangerous restriction or mask the return of compensatory behaviors. The consistent pattern we observe is that patients with prior restrictive or binge-type disorders do best when semaglutide is prescribed only after a coordinated plan with an eating-disorder specialist, a nutritionist, and a therapist.
That plan should include measurable goals that are not purely weight-based, scheduled meals, exposure to normal hunger cues, and weekly check-ins for the first two months. Red flags that require stopping the drug include growing preoccupation with food, orthostatic symptoms from low intake, or increasing use of laxatives or diuretics.
How Does Semaglutide Interact With Gallbladder, Pancreas, And Kidney Conditions?
Semaglutide slows gastric emptying and changes biliary dynamics, which can increase gallstone formation and exacerbate biliary colic in susceptible people. If you have gallbladder disease but are not an automatic exclusion, baseline abdominal imaging and a plan for early evaluation of biliary pain make the difference between a managed trial and an avoidable emergency. For patients with prior pancreatitis, the risk is higher; according to MedPage Today, “10% increase in risk for those with a history of pancreatitis.”
Prior pancreatic injury increases the risk of recurrence; therefore, gastroenterology involvement and close enzyme monitoring are mandatory when a trial is considered. Kidney disease changes the equation, too, because persistent vomiting or diarrhea can quickly trigger acute kidney injury; in practice, that means preplanned lab monitoring, clear hydration instructions, and criteria for dose holds if creatinine or electrolytes shift.
What About Hypersensitivity and Unusual Allergic Reactions?
Some patients experience severe allergic responses when exposed to peptide injectables. The safe approach is to document any prior anaphylactic episodes, review other injectable allergies, and ensure patients know the immediate signs of an allergic reaction. For those without prior severe allergy, a plan for urgent access to emergency care and clear instructions on when to present are simple, effective safeguards.
Will Semaglutide Change How Other Drugs Work in My Body?
Yes. Because the medication slows digestion, drugs with narrow therapeutic windows may be absorbed differently. Warfarin, certain antibiotics, oral contraceptives, and seizure medications can affect in timing or peak concentration. The practical step is to have a medication reconciliation with a pharmacist before starting, and to make specific monitoring or timing adjustments for oral medications when necessary.
How Do Clinicians Actually Make These Tradeoffs Without Guessing?
Most people manage semaglutide with ad hoc notes, calendar reminders, and sporadic lab orders because this approach is familiar and low-effort. That approach works until signals fragment: mood drops go unlogged, mild abdominal pain becomes severe, or lab schedules slip. That hidden cost leads to delayed responses and avoidable complications.
Solutions like MeAgain centralize dose schedules, let users log side effects by voice or photo, automate reminders for labs and mood checks, and flag trends, reducing the time between a concerning sign and clinical action. Teams find that with structured tracking and automated alerts, early problems are addressed within days rather than weeks, preventing many small issues from becoming treatment failures.
What Practical Monitoring Schedules Make Sense?
Use constraint-based thinking:
If psychiatric history is present, increase visit cadence from monthly to weekly during titration and add a validated screener at each contact.
If prior pancreatitis is present, check amylase and lipase at baseline, then at short, predefined intervals during dose increases and whenever abdominal pain occurs.
If stage 3 kidney disease or worse is present, measure creatinine within a few days of any persistent vomiting or diarrhea and set a low threshold for pausing treatment.
These are patterns that reduce guesswork and make decisions reproducible.
A quick analogy to make it concrete:
Semaglutide adjusts the body’s appetite thermostat, and for many people, that yields a comfortable temperature and improved function. For those with fragile controls, thermostat adjustments must be made slowly, with someone monitoring to ensure the room does not cool too quickly. According to MedPage Today, “5% of patients experienced severe side effects.” A small but real subset will develop severe reactions, so planning for early detection is not optional; it is part of safe prescribing.
What to Watch for, in One Actionable List
Establish baseline measures, including a mood scale, an abdominal exam or imaging, pancreatic enzyme levels, and renal function tests.
Increase contact frequency during titration, with simple, scheduled check-ins.
Define objective stop rules before starting: specific lab thresholds, symptom triggers, or mood score cutoffs.
Engage specialists up front when two or more risk domains overlap, for example, psychiatry plus GI.
Use structured logging and reminders so no single signal is left to memory or chance.
That uneasy sensation you’ve been carrying about whether semaglutide is safe for you is useful; it means the next step should be precise, not rushed.
Related Reading
Who Should Not Take Semaglutide
Semaglutide Eye Side Effects
Compounded Semaglutide Side Effects
Semaglutide Belly Fat
Semaglutide Visceral Fat
Liraglutide vs Semaglutide
What to Do If You’re Unsure Semaglutide Is Right for You

Deciding if semaglutide is right for you should be a collaborative medical choice, not a rushed yes or no. You and your clinician need clear goals, a realistic timeline, and an agreed-upon monitoring plan that tracks both benefits and harms.
What Should I Bring to the Appointment?
Bring a concise, clinical packet: a one-page timeline of your weight history and prior strategies; a current medication list with doses; recent lab results, if available; and a brief symptom log for two weeks showing appetite, bowel habits, sleep, and mood. When we reviewed patient intake routines across clinics, the patients who benefited most arrived with this exact information, enabling clinicians to turn a 20-minute visit into a focused decision rather than guesswork. Also note your priorities beyond pounds, for example, improving energy, reducing medication for high blood pressure, or lessening food preoccupation, because those goals shape what “success” looks like clinically.
How Should I Track Response and Side Effects?
Use simple, repeatable measures you can share. We recommend daily single-number ratings for hunger, nausea, mood, and energy, plus one line noting bowel frequency and consistency. Expect early appetite changes, and be prepared. More than 50% of users reported reduced appetite in the first month.
Check-in cadence matters:
Capture daily data for the first four weeks, then summarize weekly for the next two months.
Build objective stop or pause rules before you start, for example, sustained nausea or vomiting lasting more than 48 hours, a mood score drop of four or more points from baseline combined with any suicidal thoughts, or new severe constipation unresponsive to standard measures.
These rules turn anxiety into action, so you and your clinician can stop or adjust treatment quickly and safely.
Who Should Be on My Team, and How Will Decisions Be Made?
If you have complex medical issues, assemble a named team:
primary care
Endocrinology or obesity medicine
Registered dietitian
Mental health clinician
When there is a psychiatric history. For specific organ risks, add the appropriate specialist.
The clinical pattern to see is clear:
When two or more risk domains overlap, frequent scheduled contacts during titration reduce preventable problems. Frame decisions as checkpoints, not forever judgments: trial for 12 weeks with predefined metrics, then choose continue, adjust, or stop based on that data.
What About Alternatives, Costs, and The Real-World Tradeoffs?
Semaglutide can produce meaningful results, and that matters clinically, but it is not the only route. Consider stepwise options:
Intensify lifestyle with structured behavioral therapy.
Try other pharmacotherapies when appropriate.
Refer for procedural options when indicated.
Financial planning should be part of the medical conversation, too, because affordability affects adherence and outcomes. Ask your clinician for cost estimates, prior authorization pathways, and assistance programs before you start. Expectation management pays off; knowing how long you will commit, what follow-up looks like, and what counts as success keeps decisions humane and practical.
Closing the Gap Between Scattered Notes and Faster Clinical Action
Most people initially manage their doses, symptoms, and labs with scattered notes, which works until signals fragment. As doses change, missed labs and vague symptom reports become hidden costs that delay adjustments and increase risk. Solutions like MeAgain share that familiar approach, reveal how fragmentation delays clinical action, and provide a bridge by centralizing personalized plans, automated scheduling, simple speak-or-scan logging, and side-effect trend alerts, so clinicians and patients can act faster and with confidence.
How Should I Weigh Benefit Against Harm for My Situation?
Put numbers next to feelings. Use the monitoring plan to answer two specific clinical questions at 8 to 12 weeks: whether appetite or metabolic markers have shifted enough to justify continuing, and whether side effects are tolerable with conservative management.
Remember that meaningful weight change is possible, but it is not guaranteed; according to Approximately 70% of patients reported significant weight loss after 6 months of using semaglutide that efficacy should be balanced against the lived experience see often, where patients celebrate reduced food noise and clearer eating decisions but still need follow-up for persistent symptoms such as chronic constipation or lingering pain that medication alone did not solve.
What Will Give Me Confidence to Decide Well?
Treat the first 12 weeks as a diagnostic trial with measurable goals, named stop rules, and a team that reviews the data regularly.
Track appetite, mood, bowel function, injection adherence, and labs in a single place so patterns are visible, not buried.
That way, starting or stopping medication is not emotional; it is clinical: evidence guiding a shared decision toward long-term health and safety. That choice feels heavy now, but the next step reveals the practical tools and daily habits that turn uncertainty into steady progress.
Make Safer, Smarter Progress on Semaglutide with MeAgain
Building on the monitoring checklist above, if you are weighing semaglutide and want the decision to be clinical rather than emotional, we should turn scattered notes into a clear, shared record you can act on. Most people default to ad hoc tracking that lets contraindications or emerging mood and digestive warning signs slip through, and platforms like MeAgain centralize personalized plans, smart scheduling, speak or scan logging, side-effect trend alerts, and a friendly capybara guide so you and your clinician can detect trouble early and make safer, confidence-based decisions.
Our app helps you:
Stay on top of protein, fiber, hydration, and movement to reduce common side effects
Monitor how your body responds so you can notice issues early and talk to your provider
Avoid pitfalls like muscle loss, constipation, or burnout that can derail progress
Track milestones with your Journey Card so your transformation stays intentional, not rushed
With our playful capybara guide, MeAgain turns responsible GLP-1 use into something sustainable and even enjoyable. Download MeAgain to make your weight-loss journey safer, smarter, and more supportive of your long-term health.
Related Reading
• What to Do When Semaglutide Stops Working
• How Can I Track My Semaglutide Progress?
• How Much Protein Should I Eat on Semaglutide
• How to Track My Semaglutide Side Effects?
• How to Track My Injections on Semaglutide?
• Semaglutide for Weight Loss in Non-Diabetics Dosage
• Semaglutide Body Composition
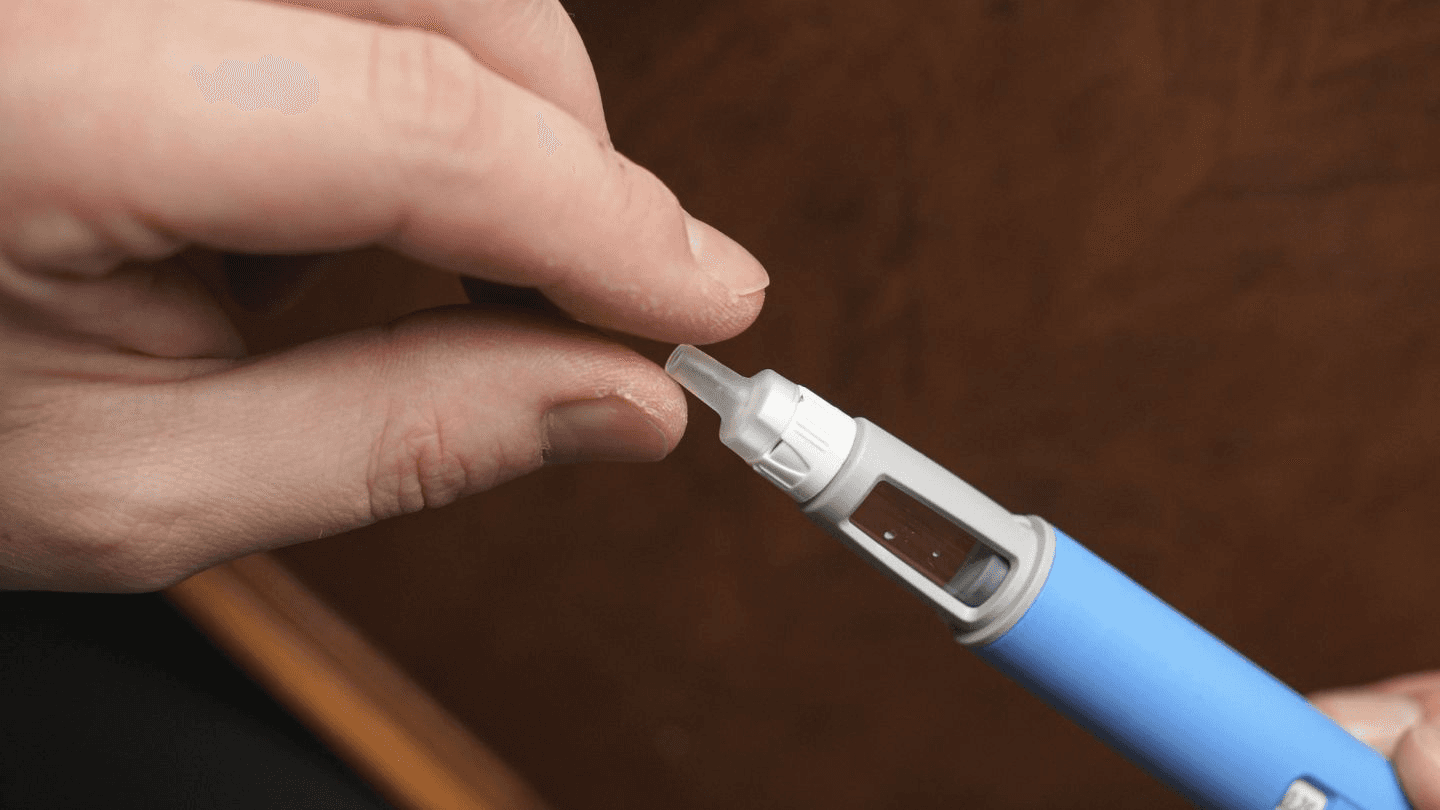
• How to Inject Semaglutide
• Best App for Tracking Semaglutide Results
• Semaglutide Foods to Avoid
• How to Track Food on Semaglutide

